Antibiotic Comparison Tool
Compare Antibiotics
Explore the key differences between ampicillin, amoxicillin, and penicillin G across clinical attributes.
| Attribute | Ampicillin | Amoxicillin | Penicillin G |
|---|---|---|---|
| Spectrum | Broad (Gram-positive + many Gram-negative) | Broad (better oral absorption) | Narrow (mostly Gram-positive) |
| Key Organisms | E. coli, H. influenzae | E. coli, H. influenzae | Streptococci, Staphylococci |
| Oral Administration | ~20% | ~90% | Poor (IV/IM only) |
Key Insight: Ampicillin expanded treatment options for Gram-negative infections like E. coli and H. influenzae, which penicillin G couldn't effectively treat.
| Attribute | Ampicillin | Amoxicillin | Penicillin G |
|---|---|---|---|
| Oral Bioavailability | ~20% | ~90% | Poor |
| Typical Adult Dose | 250-500 mg Q6-8h | 250-500 mg Q8h | 1-2 million U IV q4h |
| Route of Administration | Oral, IV | Oral | IV, IM |
Key Insight: Amoxicillin's superior oral bioavailability (90% vs. 20% for ampicillin) made it more practical for outpatient treatment.
| Attribute | Ampicillin | Amoxicillin | Penicillin G |
|---|---|---|---|
| Primary Resistance Mechanism | β-lactamase production | β-lactamase, altered PBPs | β-lactamase, low affinity PBPs |
| Resistance Risk | High | High | High |
| Resistance Mitigation | β-lactamase inhibitors | β-lactamase inhibitors | Not applicable |
Key Insight: All three antibiotics face β-lactamase resistance, but ampicillin and amoxicillin can be combined with inhibitors like clavulanate to overcome this.
- Enterococcal endocarditis
- Meningitis (susceptible strains)
- Respiratory infections
- Urinary tract infections
- Otitis media
- Sinusitis
- Community-acquired pneumonia
- UTIs
- Streptococcal infections
- Syphilis
- Staphylococcal infections (penicillin-sensitive)
- Rheumatic fever prophylaxis
Key Insight: Ampicillin remains important for enterococcal infections, while amoxicillin has largely replaced it for many outpatient infections due to better oral absorption and tolerability.
Quick Takeaways
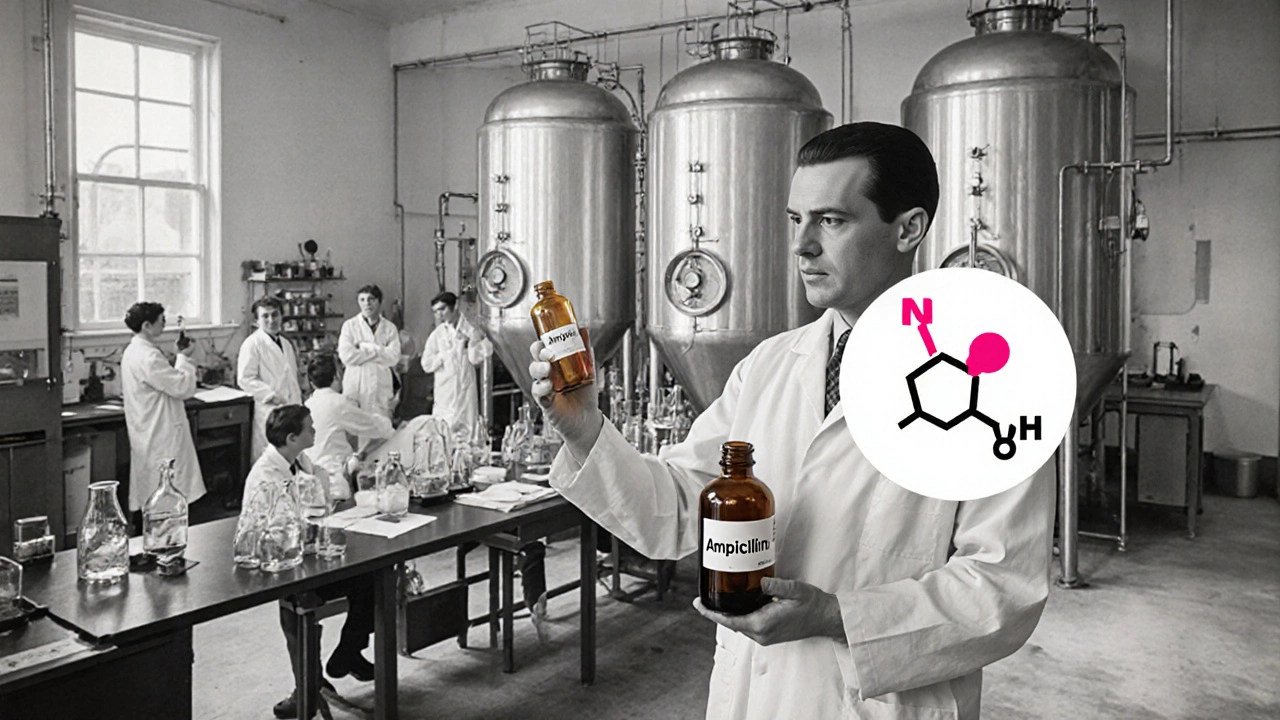
- Ampicillin was introduced in the early 1960s as the first broad‑spectrum penicillin derivative.
- It emerged from research on the β‑lactam ring discovered by Sir Alexander Fleming and Sir Ernst Chain.
- The drug’s development involved Pfizer’s large‑scale fermentation and chemical modification techniques.
- Ampicillin reshaped treatment of respiratory, urinary, and meningitis infections.
- Resistance rose quickly, prompting the rise of newer agents like amoxicillin and β‑lactamase inhibitors.
When doctors first faced the limits of narrow‑spectrum penicillins, a new champion stepped onto the scene. Ampicillin is a semi‑synthetic β‑lactam antibiotic that extended the reach of penicillin to many Gram‑negative bacteria, dramatically expanding treatment options for hospitals worldwide.
The story of ampicillin isn’t just about a single molecule; it’s a snapshot of post‑World WarII science, industry, and public health. From the labs of the United Kingdom to the fermentation vats of American drug makers, the drug’s journey reflects how collaboration and urgency can reshape medicine.
Origins of the β‑Lactam Family
The foundation of ampicillin lies in the discovery of the β‑lactam ring. In 1928, Sir Alexander Fleming noticed a mold killing bacteria on a petri dish, leading to the isolation of penicillin. Sir Ernst Chain and his team later elucidated the molecule’s structure, revealing the crucial four‑membered β‑lactam ring that interferes with bacterial cell‑wall synthesis.
While penicillin G was a wonder drug, its effectiveness was confined mostly to Gram‑positive organisms. Scientists soon realized that tweaking the penicillin nucleus could broaden the spectrum. The term “β‑lactam antibiotics” now covers a whole class-including penicillins, cephalosporins, carbapenems, and monobactams-linked by that same four‑atom ring.
From Penicillin to Ampicillin: The Chemical Leap
By the mid‑1950s, researchers at the Pfizer research facility in New York were experimenting with side‑chain modifications. Their goal: attach a broader‑spectrum side group to the penicillin core without losing the β‑lactam’s bacterial‑killing power.
In 1961, the team succeeded with a para‑amino phenyl side chain, creating ampicillin (originally named “Bristol‑Meyers”). This new molecule retained the essential β‑lactam ring while gaining the ability to cross the outer membrane of many Gram‑negative bacteria, such as Escherichia coli and Haemophilus influenzae. The result was the first truly broad‑spectrum penicillin.
Clinical Trials and Early Adoption
After pre‑clinical success, ampicillin entered human trials in 1962. The PhaseIII studies, conducted across hospitals in the United States and Europe, focused on three key infection types:
- Respiratory tract infections (pneumonia, bronchitis)
- Urinary tract infections caused by Klebsiella andProteus species
- Meningitis caused by susceptible strains of Neisseria meningitidis
Results showed cure rates of 85‑90%-a significant improvement over narrow‑spectrum penicillins. By late 1964, the FDA approved ampicillin for intravenous and oral use, and it quickly became a staple in hospital formularies.
Impact on Medical Practice
Ampicillin’s introduction reshaped empiric therapy protocols. Doctors could now start a patient on a single drug while awaiting culture results, reducing the need for multiple narrow‑spectrum agents and shortening hospital stays. Its oral formulation (ampicillin sodium) made community treatment of sinusitis and otitis media more feasible.
Public health agencies, such as the World Health Organization, listed ampicillin in their Essential Medicines List (first inclusion in 1977). This recognition underscored its global importance, especially in low‑resource settings where intravenous therapy options were limited.
Resistance Emerges: The Arms Race Begins
Unfortunately, the broader spectrum also spurred bacterial resistance. Within a decade, β‑lactamase-producing strains of Staphylococcus aureus and Enterobacter eroded ampicillin’s efficacy. Researchers responded by developing β‑lactamase inhibitors (e.g., sulbactam) and newer penicillins like Amoxicillin, which offered improved oral bioavailability and resistance profiles.
The rise of resistance transformed how clinicians think about antibiotic stewardship. Guidelines now emphasize narrow‑spectrum agents whenever possible and reserve broad‑spectrum drugs like ampicillin for proven indications.

Comparing Ampicillin with Modern Penicillins
| Attribute | Ampicillin | Amoxicillin | PenicillinG |
|---|---|---|---|
| Discovery year | 1961 | 1972 | 1928 |
| Spectrum | Broad (Gram‑positive + many Gram‑negative) | Broad (better oral absorption) | Narrow (mostly Gram‑positive) |
| Oral bioavailability | ~20% | ~90% | Poor (requires IV/IM) |
| Typical daily dose (adult) | 250-500mg Q6‑8h | 250-500mg Q8h | 1‑2millionU IV q4h |
| Common resistance mechanisms | β‑lactamase production | β‑lactamase, altered PBPs | β‑lactamase, low affinity PBPs |
While ampicillin remains useful for specific infections (e.g., enterococcal endocarditis), many clinicians now prefer amoxicillin or combination regimens that include a β‑lactamase inhibitor for better oral coverage and resistance mitigation.
Legacy and Future Directions
The development of ampicillin taught the pharmaceutical industry a vital lesson: extending a drug’s spectrum can be a double‑edged sword. The molecule paved the way for a generation of β‑lactam antibiotics, influencing synthetic strategies, formulation science, and regulatory pathways.
Today, research focuses on reviving older β‑lactams by pairing them with novel inhibitors or using nanocarrier delivery to bypass resistance mechanisms. Some experimental programs even explore engineered β‑lactamases that can degrade toxic bacterial metabolites, turning a resistance factor into a therapeutic advantage.
In the classroom, ampicillin serves as a case study in drug design, illustrating how a simple chemical tweak-adding an amino‑phenyl side chain-can transform medical practice worldwide.
Frequently Asked Questions
When was ampicillin first approved for medical use?
The U.S. Food and Drug Administration gave its first approval in 1964, authorizing both intravenous and oral formulations for a range of bacterial infections.
How does ampicillin differ from penicillin G?
Ampicillin carries an amino‑phenyl side chain that expands its activity to many Gram‑negative organisms and allows limited oral administration, whereas penicillin G is primarily effective against Gram‑positive bacteria and is administered intravenously or intramuscularly.
Why did resistance to ampicillin appear so quickly?
Bacteria that produce β‑lactamase enzymes can hydrolyze the β‑lactam ring, rendering ampicillin ineffective. The widespread use of the drug created strong selective pressure, accelerating the spread of these resistant strains.
Is ampicillin still used in modern clinical practice?
Yes, especially for infections caused by susceptible Enterococcus species, certain meningitis cases, and when a clinician needs a reliable IV agent with a known safety profile. However, many practitioners favor newer penicillins or β‑lactamase inhibitor combos for broader coverage.
Can ampicillin be taken during pregnancy?
Ampicillin is classified as a Category B drug by the FDA, meaning animal studies have shown no risk and there are no well‑controlled studies in pregnant women. It is generally considered safe when the benefits outweigh potential risks.






Posts Comments
rama andika October 15, 2025 AT 12:31
Oh sure, the “heroic” saga of ampicillin is just another chapter in the grand pharma‑conspiracy playbook. They conveniently gloss over how the same corporations that pushed penicillin later rushed ampicillin onto shelves, ignoring the inevitable fallout. If you look past the glossy press releases, you’ll see a pattern of profit‑driven shortcuts.
Kenny ANTOINE-EDOUARD October 20, 2025 AT 18:31
While the tone above is certainly colorful, the historical record shows a more nuanced picture. Ampicillin was indeed a milestone, emerging from decades of β‑lactam research that began with Fleming’s accidental mold discovery in 1928. The structural modification-a para‑amino phenyl side chain-allowed the molecule to penetrate the outer membrane of many Gram‑negative bacteria, something penicillin G could not achieve. Pfizer’s fermentation breakthroughs in the late 1950s provided the bulk drug substance at a scale previously unimaginable, which in turn made clinical trials feasible. The Phase III trials of 1962‑1964 demonstrated cure rates approaching 90 % for pneumonia, urinary tract infections, and meningitis, a dramatic improvement over earlier narrow‑spectrum agents. FDA approval in 1964 opened the door for both intravenous and oral formulations, expanding therapeutic options beyond the hospital setting. However, the rapid uptake also created a selective pressure that accelerated the emergence of β‑lactamase‑producing organisms. By the early 1970s, resistance patterns forced clinicians to reconsider empiric monotherapy with ampicillin alone. This led to the development of β‑lactamase inhibitors such as sulbactam and the introduction of amoxicillin, which offered superior oral bioavailability. The story of ampicillin thus illustrates a classic arms race: a drug expands the therapeutic arsenal, bacteria adapt, and new drugs become necessary. From a pharmacoeconomic standpoint, ampicillin’s relatively low cost contributed to its inclusion on the WHO Essential Medicines List in 1977, benefiting low‑resource health systems worldwide. Contemporary stewardship guidelines now recommend reserving broad‑spectrum agents for proven indications, reflecting lessons learned from the early days of ampicillin use. Moreover, modern research is revisiting older β‑lactams, pairing them with novel inhibitors or nanocarrier systems to overcome resistance mechanisms. Such approaches echo the original spirit of innovation that birthed ampicillin, reminding us that drug development is an iterative process. In educational settings, ampicillin serves as a case study for medicinal chemistry, illustrating how a single side‑chain alteration can transform clinical practice. Ultimately, while the narrative contains elements of corporate ambition, it also showcases genuine scientific advancement that saved countless lives.
Jessica Wheeler October 26, 2025 AT 00:31
The reckless overuse of any antibiotic is a betrayal of our duty to future patients.
Sinead McArdle October 31, 2025 AT 05:31
I appreciate the sentiment, and it aligns with current stewardship policies that stress narrow‑spectrum use whenever feasible. Maintaining discipline in prescribing helps preserve efficacy for those who truly need it.
Katherine Krucker Merkle November 5, 2025 AT 11:31
Ampicillin’s role in treating community‑acquired sinusitis really paved the way for oral outpatient therapy. Its modest oral bioavailability, though lower than amoxicillin, still allowed physicians to avoid hospital admissions in many cases. It’s interesting to see how that early success shaped today’s preference for amoxicillin‑clavulanate in similar infections.
Mark Quintana November 10, 2025 AT 17:31
thats true, but remember that ampicillin still has a place in enterococcal endocarditis treatment. it's just less favoured becaus of the resistance issues.
Brandon Cassidy November 15, 2025 AT 23:31
Indeed, the choice between historical agents and newer combos reflects a deeper trade‑off between proven safety and evolving resistance patterns. One could argue that preserving older drugs requires a collective ethical commitment.
Taryn Esses November 21, 2025 AT 05:31
Ampicillin helped a lot before resistance got so bad. It saved many kids from meningitis back then.
Albert Lopez November 26, 2025 AT 11:31
The nostalgia you express overlooks the fact that reliance on a single drug fostered a predictable evolutionary response in pathogens. Intellectual honesty demands we critique that short‑sightedness.
Erica Harrington December 1, 2025 AT 17:31
Great points all around-especially the reminder that stewardship isn’t just a buzzword, it’s a practical necessity. Let’s keep pushing for education about proper dosing and duration. Together we can curb resistance trends.
Patricia Mombourquette December 6, 2025 AT 23:31
Education alone won’t suffice; policy enforcement is essential.
karl lewis December 12, 2025 AT 05:31
From a philosophical standpoint, the entire saga of ampicillin illustrates the paradox of progress: each breakthrough begets a new problem, demanding yet another solution. One could lament the endless cycle, yet also celebrate humanity’s relentless ingenuity. In the end, the drug’s legacy is both a cautionary tale and a testament to scientific perseverance.
Amy Martinez December 17, 2025 AT 11:31
Your reflection captures the bittersweet beauty of medical innovation, reminding us that every triumph carries a shadow. It’s moving to see such reverence for the scientists who dared to tweak a humble molecule. May their spirit inspire us to craft smarter, kinder therapies.
Write a comment