Imagine one small pill helping you tackle two stubborn causes of high blood sugar at once. That’s the power that Glucovance brings to the table for people fighting type 2 diabetes. It’s not a magic bullet, but it’s got a track record that’s impossible to ignore—especially if you’ve ever felt like your diabetes treatment is a never-ending juggling act. Glucovance takes two classic diabetes meds, glyburide and metformin, and combines them into a single tablet. Simple, right? But why should you care, and what’s hiding behind that tiny combo pill?
What Exactly is Glucovance? Breaking Down the Combo
Glucovance isn’t just any old diabetes medication. It’s a blend of two heavy hitters: glyburide and metformin. Metformin’s been around since the 1950s. It helps your liver chill out on pumping too much sugar into your blood, and also helps your muscles use sugar better. Think of it as a behind-the-scenes manager. Glyburide, on the other hand, is a type of medicine called a sulfonylurea. It tells your pancreas to work a little harder to pump out more insulin. Together, they make this ‘dynamic duo’ that knocks down blood sugar from two directions.
That’s the technical side, but what does it mean for you? Having both drugs in one pill cuts down on the number of meds you need to take. No more keeping track of which pill to swallow when. Plus, studies show Glucovance controls blood sugar more steadily for a lot of folks who don’t do well on just one drug alone.
Pharmacists notice something else: when people have fewer pills to remember, they actually stick to their treatment better. Real talk—missing a dose happens. Life happens. But taking just one pill, once or twice a day—most people find that easier to remember. And that, in the end, can mean better blood sugar numbers and fewer diabetes roller coasters.
Let’s get even more specific. Glucovance comes in different strengths, to fine-tune just for you and your blood sugar targets. The usual starting dose is 1.25 mg of glyburide with 250 mg of metformin, but it can go up, always under your doctor’s watch. It can be taken once or twice daily with meals to prevent stomach upset. Always eat before you take it, trust me—otherwise, you’re cruising for a queasy day.
Some people wonder if Glucovance is right for type 1 diabetes or if they’re pregnant. The answer is simple: it’s FDA-approved specifically for type 2 diabetes in adults, and it’s a no-go for type 1, anyone with diabetic ketoacidosis, or pregnancy. Always keep your doctor in the loop if you’re thinking about switching or starting Glucovance.
One quick tip: keep water handy. Metformin is known to upset the stomach, especially at first, but chasing your pill with plenty of water and never taking it on an empty stomach can help a lot. If you’re already taking either glyburide or metformin alone and your numbers aren't at goal, you might hear your doctor mention Glucovance as your next step.

Risks, Side Effects, and What to Watch Out For
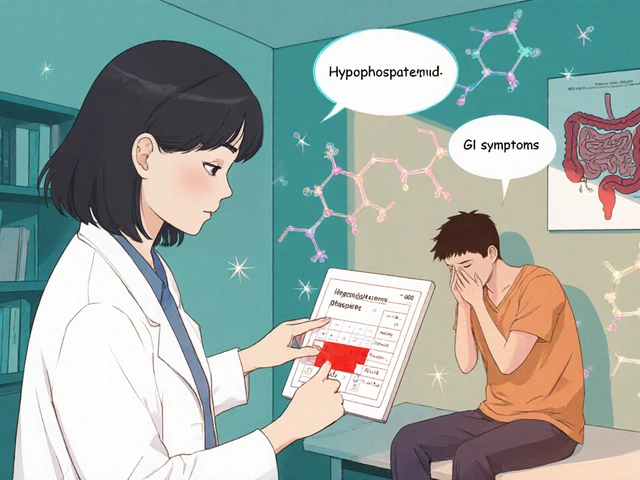
Every medicine has a flip side. For Glucovance, the most talked-about downsides come from both ingredients. Glyburide packs a punch, and sometimes your blood sugar can swing too low—hello, hypoglycemia. Metformin, on the other hand, can make your stomach cranky. Most folks feel this as diarrhea, queasiness, or a metallic taste, especially in the first weeks as their body gets used to the new routine.
If you’re reading this and thinking "I already have a sensitive stomach," heads up. The trick is to always eat before you take Glucovance, and never skip meals. Skipping food plus glyburide equals a bigger risk for low blood sugar—and those lows can sneak up fast. Symptoms can include sweating, racing heart, shaking, or feeling super hungry out of nowhere. Keep a source of quick sugar handy—like glucose tabs or juice—for emergencies.
Rarely, metformin can cause a condition called lactic acidosis. This sounds scary because it is—it happens when your body builds up too much lactic acid. Symptoms are subtle at first: deep or rapid breathing, unusual sleepiness, stomach pain, or feeling faint. It’s super rare (about 1 in 30,000 people per year), but it’s worth knowing about so you can call for help if you ever notice these signs.
Now, let’s talk long-term. Glyburide can stress your pancreatic cells after years of use—meaning, eventually, your pancreas might get tired out and not make as much insulin as it used to. That’s normal for type 2 diabetes progression, but it means you and your provider may need to revisit your meds now and then. Metformin, over years, might cause your vitamin B12 levels to drop. If you feel extra tired, numb, or tingly, ask about checking B12 next time you see your doctor.
Certain people need to think twice before taking Glucovance. If you have kidney or liver problems, this combo might not be safe for you. There’s a reason doctors check your labs before starting you on it. Glucovance shouldn’t be started if your kidneys aren’t up to snuff, because metformin and glyburide both clear out through them. Most guidelines suggest avoiding Glucovance if your estimated glomerular filtration rate (eGFR) drops below 60 mL/min/1.73 m². This is something your doctor checks with a simple blood test.
Mixing Glucovance with certain other medications or alcohol can raise your risk for low blood sugar or that rare lactic acidosis. Common culprits are blood pressure pills like beta-blockers, certain antibiotics, or even over-the-counter pain relievers. When in doubt, ask your pharmacist to do a quick check—better to be safe than sorry.
If you ever need to have contrast X-rays—like CT scans with dye—let your care team know you’re on Glucovance. Metformin needs to be stopped temporarily before and after the procedure until your kidneys are checked again. It sounds like a hassle, but skipping this step could save you a world of trouble.
Allergic reactions are rare but possible with any med. If you notice a skin rash, trouble breathing, or swelling in your face or throat after starting Glucovance, call for help right away.
Bottom line: most people do fine with Glucovance, especially if they ease into their dose and keep an eye on their kidneys, sugars, and vitamin levels. But this isn’t a “set it and forget it” prescription. Keep track of any weird symptoms and keep those regular doctor appointments on your calendar.

Real-World Tips, Alternatives, and What to Ask Your Doctor
Lifestyle matters more with Glucovance than some folks expect. The combo pill works best when you pair it with healthy eating and moving more. Small changes—like swapping out sugary drinks for water, or adding a walk after dinner—boost the power of any diabetes medicine, Glucovance included. Your results will always look better when you stick to a plan you actually like, not something that feels like punishment.
Medications like Glucovance aren’t the only option out there. If you run into side effects that just won’t quit, or your blood sugar starts to climb again after months or years, there are other combos and newer classes available. Sitagliptin/metformin, empagliflozin/metformin—the list goes on. Some are easier on the stomach, others help with weight loss, and some carry a lower risk of hypoglycemia. No two people respond exactly the same, so don’t hesitate to ask your doctor if it’s time to revisit your treatment plan.
Cost often blindsides people, so ask up front. Glucovance, as a brand-name pill, isn’t as cheap as generics, but many pharmacies stock affordable generic versions under the names glyburide/metformin or metformin/glyburide. These work just the same. Most insurance plans cover them, especially if single-agent pills alone didn’t do the trick for your A1c goals. Just double-check your plan or ask your pharmacist—they can cut through the red tape.
If you’re the kind of person who likes to keep an eye on your numbers, a home blood sugar meter is a must-have. Test when you feel off, and track your results to spot patterns. Your doctor will probably want to check your A1c every three to six months too. Have your numbers handy at each visit—it helps make better decisions for your long-term health.
Here’s something most folks don’t expect: life can throw you curveballs, like a bad cold or a stomach bug. If you’re vomiting, can’t eat, or your blood sugar drops too low, talk to your care team before taking Glucovance. Sometimes it’s safer to pause until you’re better—missing a day or two won’t be the end of the world, but ignoring symptoms can set you up for trouble.
Keep in mind, Glucovance is not for weight loss, but it won’t usually pack on pounds either if you mind your diet and activity. Some people do notice a small drop in weight from the metformin side. Stay patient: changes won’t happen overnight, but steady progress always beats quick fixes that burn out fast.
If you’re worried about your kidneys, heart, or anything else, get to know your numbers: eGFR, A1c, cholesterol. These are the building blocks of better diabetes care, and knowing your baselines puts you in the driver’s seat. Never be afraid to ask, "What should I watch for?" or "What are my options if I feel lousy on this med?" Most providers appreciate the chance to partner with someone who takes their health into their own hands.
In the end, Glucovance is a powerful tool when diet and exercise alone fall short. It brings together two proven medications, cuts down pill burden, and helps smooth out those infamous blood sugar swings. But it’s not a “one size fits all,” so keep talking to your care team, track your numbers, and make changes when you need to. Diabetes management is rarely a straight path. Glucovance might be the right fork in the road for you, or maybe just one stop along the way.





Posts Comments
Asha Jijen June 27, 2025 AT 23:16
glucovance just saved my life no more 5 pills a day and my sugar is stable i cant believe i waited so long to switch
Tom Shepherd June 28, 2025 AT 19:05
i started glucovance last month and my stomach still feels like its hosting a riot. im on the lowest dose but the metallic taste is unreal. anyone else get this or am i just cursed?
marie HUREL June 29, 2025 AT 00:37
i was skeptical at first but the combo really does make a difference. i used to forget one pill or take them at the wrong time, now i just take one with breakfast and one with dinner. my a1c dropped from 8.2 to 6.9 in four months. not magic, but it works. also, drink water. lots of it. it helps with the nausea.
Frances Melendez June 30, 2025 AT 14:22
people act like this is some miracle drug but honestly its just another way to keep you dependent on pharma. why not just eat real food and move? i know people who reversed their diabetes with keto and fasting. glucovance is just a bandaid with side effects.
Rebecca Price July 2, 2025 AT 13:03
Frances, i hear you-lifestyle changes are foundational. but let’s not pretend that everyone has the time, resources, or metabolic resilience to "just eat real food." For many of us, glucovance is the bridge between survival and stability. And yes, it’s a tool-not a cure-but it’s one that lets people live longer, more functional lives. That’s not weakness. That’s science meeting reality.
Sue Haskett July 4, 2025 AT 04:56
Tom, you’re not cursed-metformin’s metallic taste is SO common, especially at first. Try brushing your teeth right after taking it, or use a straw for water. Also, switching to the extended-release version might help-less GI chaos. And yes, it’s annoying, but it’s way better than diabetic neuropathy. Trust me, I’ve been there.
Jonah Thunderbolt July 4, 2025 AT 17:07
Let’s be real: glucovance is the Ferrari of combo pills. 🚗💨 Glyburide + metformin? Classic. Elegant. Effective. Sure, your stomach might throw a tantrum for the first two weeks, but once your body stops treating it like an intruder, you’ll wonder how you ever survived on single agents. And yes, I’ve checked my B12. It’s fine. Because I’m proactive. Unlike some people who think keto is a cure-all. 🙄
Write a comment