It’s the same pill. Same active ingredient. Same dosage. Same manufacturer, sometimes. But if you open the bottle and see generic printed on the label, your body might react differently - not because of chemistry, but because of belief.
Same Medicine, Different Mindset
You’ve probably been told that generic drugs are just as good as brand-name ones. And scientifically, that’s true. The FDA requires generics to match the brand in strength, safety, and effectiveness. But here’s the catch: patients don’t always believe it. A 2019 study in the European Journal of Public Health gave 72 people identical placebo pills. Half were told they were getting a brand-name drug. The other half were told they were getting a generic. Both groups received the exact same sugar pill. But after seven days, 54% of those who thought they were taking a generic stopped taking it. Only 33% of the brand-name group did. Even though nothing in the pill changed, the label made all the difference. This isn’t magic. It’s psychology. The way a drug is labeled triggers something called the labeling effect - where your expectations shape your experience. If you think a pill is cheap or low-quality, your brain may interpret even minor discomfort as a side effect. Or worse, it may convince you the drug isn’t working at all.Placebo Power - Even Without the Active Ingredient
In another study, researchers gave students ibuprofen pills labeled as either brand-name or generic. Some pills were real. Others were placebos. The results were startling. When people took a placebo labeled as brand-name, they reported nearly the same pain relief as those who took real ibuprofen. But when the placebo was labeled generic? Pain relief dropped by almost half. The brand-name label made a sugar pill feel like medicine. The generic label made real medicine feel like nothing. Even side effects changed. More people reported nausea, dizziness, or headaches when they thought they were taking a generic - even when the pill was completely inert. The label didn’t just change perception. It changed physiology. This isn’t just about pain. It applies to anxiety meds, antidepressants, blood pressure drugs - anything where the mind plays a role in healing. Your brain doesn’t know the difference between a branded tablet and a generic one. But your beliefs? They do.Who Gets Hit Hardest?
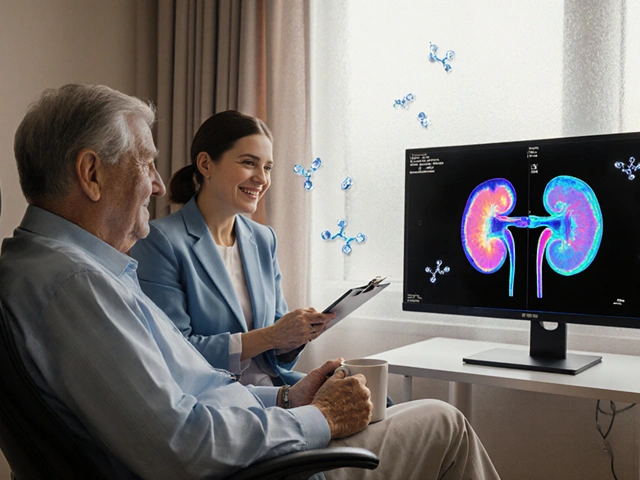
Not everyone reacts the same way. The labeling effect hits harder for people with lower health literacy. In the same 2019 study, patients who didn’t understand medical terms were 67% more likely to quit taking their generic medication than those with higher literacy. That’s not about intelligence. It’s about trust. Older adults, people on multiple medications, and those with chronic conditions like hypertension or diabetes are especially vulnerable. They’re already juggling pills, schedules, and side effects. When they see a generic label, they might assume it’s weaker - and stop taking it. That’s dangerous. Half of all patients with long-term illnesses don’t take their meds as prescribed. The labeling effect makes that number worse. And it’s not just patients. Doctors and pharmacists have biases too. A 2022 survey found that 63% of pharmacists had been asked by patients or doctors: “Is this generic really the same?” That’s not a question about science. It’s about fear.
When Labels Lie - Even When They’re Technically Correct
Here’s another problem: the labels themselves aren’t always consistent. A 2020 study looked at 31 generic drugs and compared their labels to the original brand-name versions. Every single one had differences. Some were small - font size, spacing. Others were serious. Four out of 31 had label information that could lead to life-threatening mistakes. Eleven others had risks of severe harm. Nearly half had information that could seriously affect patient safety. Why? Because when a generic drug gets approved, manufacturers aren’t required to match the original label word-for-word. They only need to prove the active ingredient is the same. The rest - warnings, dosage instructions, contraindications - can vary. Over time, these tiny differences pile up. A patient might read a generic label that says “take with food,” while the brand version says “take on empty stomach.” Confusion follows. And so does non-adherence.Cost vs. Confidence
Generics save the U.S. healthcare system about $373 billion every year. They make up 90% of all prescriptions filled. But they only account for 23% of total drug spending. That’s because people are willing to pay more for a brand name - even when they don’t need to. A 2023 Kaiser Family Foundation survey showed only 56% of Americans believe generics are as good as brand-name drugs. That’s down from 62% in 2018. People are getting more skeptical, not less. Hospitals and insurers push generics hard. Over 78% of U.S. health systems now have policies that require generics unless a doctor specifically says otherwise. But without education, those policies backfire. Patients feel tricked. They switch back to expensive brands - or stop taking meds altogether.
What’s Being Done?
Some solutions are already working. In 2020, the FDA launched “It’s the Same Medicine,” a public campaign that showed side-by-side photos of brand and generic pills with the same active ingredient. In a six-month pilot across 12 clinics, patient concerns about generics dropped by 28%. A 2023 trial added a simple phrase to generic labels: “Therapeutically equivalent to [Brand Name].” That one line cut discontinuation rates from 52% to 37%. Just telling people they’re getting the same thing - clearly and plainly - made a measurable difference. The Generic Pharmaceutical Association also launched “Generic You Can Count On” in early 2024, investing $50 million in patient education. That’s a start. But it’s not enough.What Can You Do?
If you’re a patient: Ask your pharmacist. Don’t assume the generic is worse. Ask: “Is this the same as my old pill?” They can show you the active ingredient matches. Write it down. Keep the bottle. Compare. If you’re a prescriber: Don’t just write “dispense as written” or “generic OK.” Say: “This generic is bioequivalent to [Brand Name] and approved by the FDA.” Be specific. Your words matter. If you’re a provider or insurer: Don’t just switch drugs. Explain why. Offer printed materials. Use plain language. Show pictures. Make it visual. People trust what they understand.The Bigger Picture
The labeling effect isn’t about tricking people. It’s about acknowledging that medicine isn’t just chemistry. It’s psychology too. A pill doesn’t just work because of what’s inside. It works because of what you believe is inside. We can’t stop using generics. We can’t afford to. But we can stop letting bad labels undermine them. The science is clear: the same drug, in the same dose, works the same - if you believe it does. The real question isn’t whether generics are effective. It’s whether we’re giving people the tools to believe they are.Are generic drugs really the same as brand-name drugs?
Yes, legally and scientifically. The FDA requires generic drugs to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. The only differences are in inactive ingredients (like fillers or dyes) and packaging. Bioequivalence testing ensures they work the same way in the body.
Why do some people feel generics don’t work as well?
It’s often the labeling effect - not the drug itself. When people see the word "generic," they may subconsciously expect it to be weaker or less effective. This can trigger nocebo effects, where negative expectations lead to real physical symptoms like increased pain, nausea, or fatigue. Studies show identical placebos labeled as "generic" produce weaker results than those labeled as "brand-name," even when the pill is sugar.
Can generic drug labels be misleading?
Yes. While active ingredients must match, generic labels aren’t required to mirror the original brand’s full wording. Studies found that up to 61% of generic drugs have label differences from their brand-name counterparts - some of which could cause confusion or harm. For example, dosage instructions, warnings, or contraindications might be worded differently, leading patients or providers to make incorrect decisions.
Does the labeling effect apply to all medications?
It’s strongest in conditions where perception plays a big role - like pain, anxiety, depression, and chronic fatigue. For drugs where the body’s response is purely physiological - like antibiotics or insulin - the effect is smaller. But even then, poor adherence due to distrust can lead to treatment failure. So while the mechanism varies, the outcome - missed doses, worse outcomes - is the same.
What can I do if I’m worried about my generic medication?
Talk to your pharmacist. Ask them to confirm the active ingredient matches your previous brand. Request the FDA’s "It’s the Same Medicine" fact sheet. If you notice a change in how you feel after switching, don’t assume it’s the drug. It could be your expectations. But also don’t ignore real side effects - report them. Sometimes, a different generic manufacturer may work better for you due to inactive ingredients.
Why do pharmacies switch generics without telling me?
Because multiple generic manufacturers make the same drug, and pharmacies often choose the lowest-cost option. This is legal and common. But it can cause confusion if the pills look different - color, shape, markings. That’s not a safety issue, but it can trigger the labeling effect. Always check the label for the active ingredient and ask if it’s the same as before. If you’re concerned, ask for the original brand or request the same generic manufacturer.






Posts Comments
Dikshita Mehta December 18, 2025 AT 20:28
The labeling effect is one of those quiet giants in healthcare that nobody talks about. I’ve seen patients stop their blood pressure meds because the pill looked different - not because it didn’t work, but because they thought it was ‘cheap.’ The science is rock solid, but trust isn’t built in a lab. It’s built in conversations, in clear labels, in pharmacists taking five extra seconds to explain. We need to stop treating patients like passive recipients and start treating them like partners.
pascal pantel December 20, 2025 AT 01:48
Let’s cut through the fluff. This isn’t psychology - it’s placebo nonsense dressed up as science. The FDA requires bioequivalence. End of story. If people are too dumb to understand that a pill is a pill, that’s not the system’s fault. It’s their cognitive laziness. Stop coddling patients with feel-good campaigns. Just make them take the damn generic. The system can’t afford to baby every hypochondriac who thinks their $2 pill is ‘not the same.’
Gloria Parraz December 20, 2025 AT 09:45
I’ve been a nurse for 22 years. I’ve watched people cry because they thought their generic antidepressant ‘wasn’t working.’ They weren’t lying. Their pain was real - because their belief made it real. I’ve handed out printed side-by-side comparisons of brand and generic pills. I’ve held hands while they read the active ingredient. And guess what? When they understood, the side effects vanished. It’s not magic. It’s compassion. And it’s cheaper than ER visits.
Sahil jassy December 21, 2025 AT 04:02
generic works same as brand if you believe it period no need for fancy studies just ask your pharmacist and look at the active ingredient on the bottle
Janelle Moore December 21, 2025 AT 05:31
Ever wonder why big pharma lets generics exist at all? They know people will panic over the label. That’s why they design the brand pill to look like a luxury product - the shape, the color, the logo. The generic? Looks like something you’d find in a discount pharmacy. It’s not an accident. It’s a psychological trap. And the FDA? They’re in bed with the big companies. They don’t enforce label consistency because it benefits profits. This isn’t about belief - it’s about control.
Chris porto December 21, 2025 AT 19:53
It’s fascinating how deeply our minds shape reality. A pill is just a chemical compound - until we assign meaning to it. The brand name becomes a symbol of trust. The generic? A symbol of compromise. We don’t just take medicine. We take stories. And if the story is ‘this is inferior,’ the body listens. Maybe the real breakthrough isn’t in drug development - it’s in storytelling. How do we rewrite the narrative so that ‘generic’ means ‘smart,’ not ‘cheap’?
Ryan van Leent December 22, 2025 AT 00:17
People are dumb and lazy. They don’t read the label. They don’t ask questions. They just see ‘generic’ and assume it’s trash. Meanwhile, the system saves billions and they whine about their ‘side effects’ that don’t exist. I’ve been on generics for 8 years. Never had an issue. Stop making everything a drama. Just take the pill. Your wallet and your doctor will thank you.
Adrienne Dagg December 22, 2025 AT 14:04
OMG I JUST REALIZED WHY MY ANXIETY GOT WORSE WHEN I SWITCHED TO GENERIC XANAX 😭 I THOUGHT IT WAS THE DRUG BUT IT WAS THE LABEL. I WENT BACK TO BRAND AND I’M OKAY NOW. WHY DOESN’T ANYONE TELL YOU THIS?? 🤯
Erica Vest December 22, 2025 AT 16:48
There’s a critical gap in the FDA’s approval process: label consistency. The active ingredient is regulated, yes - but warnings, contraindications, and even dosage instructions can vary wildly between brand and generic. A 2020 JAMA study found that 48% of generic labels had clinically significant wording differences. That’s not a bug - it’s a policy failure. Patients aren’t paranoid. They’re reacting to real inconsistencies. Fix the labels, not the beliefs.
Chris Davidson December 23, 2025 AT 13:14
The labeling effect is real but it is not a reason to abandon generics. The system works. The science is clear. Those who cannot accept this are not ready for modern medicine. You cannot have a healthcare system based on superstition. Take the pill. Be grateful. Move on.
Kinnaird Lynsey December 25, 2025 AT 10:22
It’s funny how we’ll spend hours researching a new phone but won’t look up the active ingredient in a pill we take daily. Maybe the problem isn’t the label - it’s that we’ve outsourced our health literacy to corporations and doctors. We don’t ask questions because we’ve been trained not to. The labeling effect? It’s just the symptom. The disease is disempowerment.
Glen Arreglo December 26, 2025 AT 01:17
I grew up in a country where generics are the norm - and people don’t question them. Why? Because the government made sure the labels were identical, the packaging was standardized, and pharmacists were trained to explain it simply. No marketing. No branding. Just facts. We didn’t need a campaign. We needed consistency. The U.S. doesn’t lack science. It lacks coordination. Fix the system, not the mindset.
Write a comment