Testosterone Replacement Therapy Calculator
Personalized TRT Dose Estimator
This tool provides general guidance for TRT dosage ranges based on medical principles. Always consult your healthcare provider for personalized treatment.
Important Medical Disclaimer: This calculator provides educational guidance only. TRT dosing must be determined by a qualified healthcare provider based on comprehensive medical evaluation, including regular monitoring of hemoglobin, hematocrit, and PSA levels.
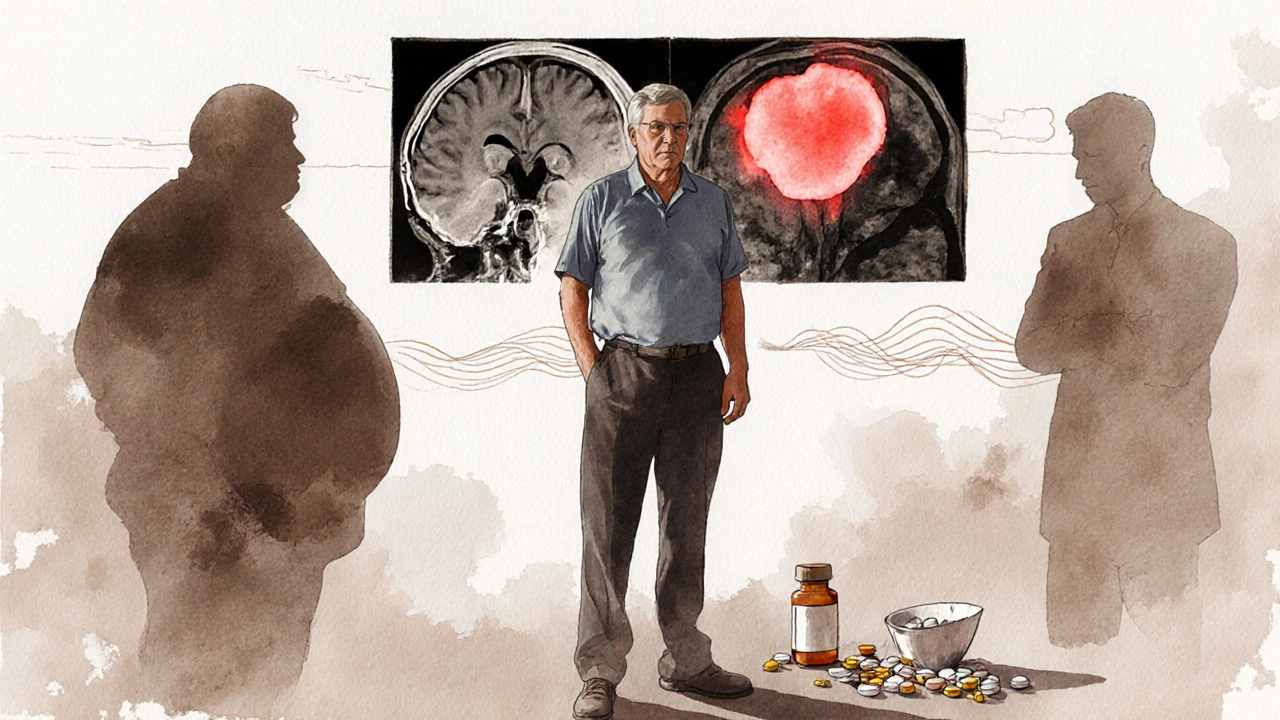
When the body’s hormone‑producing command center falters, men can end up with low testosterone even though the testes themselves are fine. That’s the core of secondary hypogonadism, a condition that often hides behind vague fatigue, reduced libido, and mood swings. Below you’ll find a straight‑talk guide that tells you what triggers the problem, how to spot it, and what you can actually do to get back on track.
Key Takeaways
- Secondary hypogonadism stems from issues in the brain’s hypothalamus‑pituitary axis, not from the testes.
- Common culprits include pituitary tumors, chronic illnesses, certain medications, and lifestyle factors such as obesity.
- Symptoms overlap with normal aging but often involve a sudden drop in energy, sex drive, and muscle mass.
- Diagnosis relies on blood tests for testosterone, LH, and FSH, plus imaging of the pituitary when needed.
- Treatment ranges from hormone replacement to addressing the underlying cause, with lifestyle tweaks boosting results.
What Is Secondary Hypogonadism?
Secondary hypogonadism is a type of testosterone deficiency that originates from a problem in the brain’s hormonal signaling pathway, specifically the hypothalamus or pituitary gland, rather than a direct issue within the testes themselves. The condition leads to low circulating testosterone because the signals that tell the testes to produce the hormone are weak or absent. The hypothalamus releases gonadotropin‑releasing hormone (GnRH), which prompts the pituitary gland to secrete luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). When either the hypothalamus or pituitary falters, LH and FSH drop, and the testes receive insufficient instruction to make testosterone.
Root Causes: Why the Signal Gets Lost
Understanding the trigger helps you target the right fix. Below is a quick rundown of the most frequent causes.
| Cause | How It Disrupts Hormone Signal | Typical Age Group |
|---|---|---|
| Pituitary Tumor | Compresses or infiltrates pituitary tissue, lowering LH/FSH output | 30‑60 |
| Chronic Illness (e.g., liver cirrhosis, HIV) | Alters cytokine balance, suppresses GnRH release | 40‑70 |
| Medication‑Induced (opioids, glucocorticoids, anti‑psychotics) | Interferes with GnRH neurons or pituitary function | Any adult |
| Obesity & Metabolic Syndrome | Elevated aromatase converts testosterone to estrogen, feeding back to suppress GnRH | 30‑50 |
| Traumatic Brain Injury | Damages hypothalamic nuclei or pituitary stalk | Young adults |
It’s worth noting that many men have more than one factor. For instance, a man with obesity who also takes chronic opioids may see a compounded drop in testosterone.
Symptoms That Might Slip Under the Radar
The signs of secondary hypogonadism often mimic normal aging, which makes self‑diagnosis tricky. Below are the most reliable clues.
- Reduced sexual desire - often the first complaint, especially if it appears suddenly.
- Erectile difficulties - not the same as vascular issues; libido loss precedes erection problems.
- Fatigue that doesn’t improve with rest.
- Loss of muscle mass and strength, despite regular exercise.
- Increased body fat, particularly around the abdomen.
- Depressed mood, irritability, or difficulty concentrating.
- Bone density reduction, leading to higher fracture risk over time.
When several of these appear together, especially in men under 50, it’s a good prompt to get checked.
How Doctors Diagnose It
Diagnosis is a step‑by‑step process that rules out primary testicular failure and pinpoints the signaling breakdown.
- Blood Test for Total Testosterone: A morning sample (7‑10am) is taken. Levels below ~300ng/dL trigger further work‑up.
- LH and FSH Levels: Low or inappropriately normal LH/FSH in the face of low testosterone points to secondary origin. Luteinizing hormone (LH) stimulates testosterone production, while follicle‑stimulating hormone (FSH) supports spermatogenesis.
- Prolactin Test: Elevated prolactin can suppress GnRH and mimic secondary hypogonadism.
- Imaging: If labs suggest a pituitary problem, an MRI of the sellar region is ordered to look for tumors or structural lesions.
- Review of Medications & Health History: Doctors compile a list of drugs, chronic diseases, and lifestyle habits that may affect hormone balance.
All these pieces together let clinicians classify the condition accurately.
Treatment Options - From Fixing the Root to Replacing the Hormone
Therapy isn’t one‑size‑fits‑all. The first goal is to address any reversible cause.
- Adjust Medications: If opioids or glucocorticoids are the culprit, doctors may taper or switch to alternatives.
- Treat Underlying Illness: Managing liver disease, HIV, or pituitary tumors (often with surgery or radiotherapy) can restore normal signaling.
- Weight Management: Losing 5‑10% body weight can lower aromatase activity, modestly raising testosterone.
If the hormonal axis can’t recover, hormone replacement steps in.
Testosterone Replacement Therapy (TRT)
TRT comes in several forms: gels, patches, injections, and pellets. The choice depends on patient preference, cost, and how quickly levels need to be normalized.
Key points to monitor:
- Serum testosterone should stay within the mid‑normal range (400‑700ng/dL).
- Hematocrit is checked every 3‑6months to avoid polycythemia.
- Prostate health is monitored with PSA levels annually.
Unlike primary hypogonadism, men with secondary forms often respond well to lower doses because the feedback loop is still partially functional.
Selective Estrogen Receptor Modulators (SERMs)
Drugs like clomiphene citrate stimulate the hypothalamus to release more GnRH, which boosts LH and FSH, indirectly raising testosterone. SERMs are popular for men who want to preserve fertility, as they don’t suppress spermatogenesis the way exogenous testosterone can.
Human Chorionic Gonadotropin (hCG)
hCG mimics LH, directly instructing the testes to produce testosterone. It’s often combined with SERMs for synergistic effect.

Lifestyle Tweaks That Support Hormone Health
Even after medical treatment, daily habits can make a noticeable difference.
- Strength Training: Resistance exercise stimulates natural testosterone spikes and improves muscle mass.
- Sleep Hygiene: Aim for 7‑9hours of quality sleep; deep REM phases are when the body releases the most testosterone.
- Balanced Diet: Include zinc‑rich foods (oysters, pumpkin seeds), healthy fats (avocado, olive oil), and limit excess sugar.
- Stress Management: Chronic cortisol elevations blunt GnRH release; mindfulness, yoga, or simple breathing exercises help.
- Limit Alcohol: Heavy drinking interferes with the hypothalamic‑pituitary axis.
These steps not only support treatment outcomes but also reduce the risk of recurrence.
When to See a Specialist
If you’ve tried lifestyle changes and still feel off‑balance, or if blood work shows low testosterone with low LH/FSH, it’s time to book an appointment with an endocrinologist or a urologist specializing in male hormone health. Early intervention can prevent long‑term bone loss and improve quality of life.
Frequently Asked Questions
Can secondary hypogonadism be reversed?
Yes, in many cases. If the underlying cause-such as a medication, pituitary tumor, or uncontrolled chronic disease-is treated, hormone levels often return to normal without the need for lifelong testosterone replacement.
Is testosterone replacement safe for men with secondary hypogonadism?
When monitored properly, TRT is safe for most men. Regular blood tests to track testosterone, hematocrit, and prostate-specific antigen (PSA) keep risks low. The key is individualized dosing and ongoing follow‑up.
Will TRT affect my fertility?
Exogenous testosterone can suppress sperm production because it reduces LH and FSH. Men who want to preserve fertility often opt for SERMs or hCG instead, or use TRT intermittently.
What’s the difference between primary and secondary hypogonadism?
Primary hypogonadism originates in the testes; LH and FSH are high because the pituitary tries to compensate. Secondary hypogonadism starts in the hypothalamus or pituitary, so LH and FSH are low or inappropriately normal.
How often should I get my hormone levels checked?
After starting any therapy, re‑check testosterone, LH, and FSH at 3‑month intervals until stable. Once stable, an annual review is usually enough, unless symptoms change.








Posts Comments
BJ Anderson October 14, 2025 AT 18:07
Secondary hypogonadism isn’t just a catch‑all for “old guys feeling sluggish”. It originates in the hypothalamus‑pituitary axis, so the testes are perfectly capable but simply never get the memo. When LH and FSH are low, the feedback loop is broken, leading to that classic triad of fatigue, loss of libido, and reduced muscle mass. Ignoring the upstream cause means you’re treating a symptom rather than the source. Understanding the neuroendocrine signal is the first step toward an effective fix.
Alexander Rodriguez October 21, 2025 AT 16:47
Most doctors start with a total testosterone test and then forget about LH and FSH, which is a big mistake. Low testosterone with low LH points straight to secondary hypogonadism, not primary testicular failure. The lab work should be done in the morning, and you need at least two measurements to confirm the trend. If the numbers line up, an MRI of the pituitary is the logical next step. This systematic approach saves time and costly misdiagnoses.
Abhinav Sharma October 28, 2025 AT 14:27
Think of the hormonal axis as a symphony 🎶 – the hypothalamus is the conductor, the pituitary is the first violin, and the testes are the brass section. When the conductor misses a cue, the whole performance falters, even though the brass players are ready. Lifestyle factors like obesity act like background noise, drowning out the conductor’s signals. Conversely, targeted weight loss or tapering off opioids can restore the rhythm without any external hormone infusion. Keep the orchestra in tune, and the music of vitality returns.
Welcher Saltsman November 4, 2025 AT 13:07
Spot on with the morning draw, and the double‑test rule is solid. I’d add that checking prolactin early can unmask a hidden pituitary adenoma that would otherwise be missed.
april wang November 11, 2025 AT 11:47
Prolactin‑secreting adenomas are a classic pitfall because they suppress GnRH, leading to low LH and FSH despite normal pituitary appearance on basic imaging. First, you need a serum prolactin level; even a modest elevation can signal a micro‑adenoma that only shows up on high‑resolution MRI. If the prolactin is markedly high, treatment with dopamine agonists like cabergoline often restores gonadal function without surgery. Second, consider the patient’s medication list – antipsychotics and certain antidepressants can raise prolactin as a side effect, and switching to a prolactin‑neutral drug may be all that’s required. Third, remember that macro‑adenomas can cause mass effect, presenting with headaches or visual field cuts, which necessitates neurosurgical consultation. Fourth, if the adenoma is small and asymptomatic, a watchful waiting strategy with periodic MRI and hormone panels can be appropriate. Fifth, lifestyle interventions such as weight reduction can lower estrogen conversion, indirectly reducing prolactin drive. Sixth, in cases where prolactin is normal but LH remains low, investigate other hypothalamic disruptors like chronic stress or severe systemic illness. Seventh, a thorough sleep assessment is worthwhile because obstructive sleep apnea can blunt hypothalamic signaling. Eighth, vitamin D deficiency has been linked to impaired pituitary output, so repletion should be on the checklist. Ninth, iron overload conditions like hemochromatosis can infiltrate the pituitary and should be screened in at‑risk populations. Tenth, for patients unwilling to pursue invasive diagnostics, a trial of low‑dose clomiphene can test the hypothalamic responsiveness before committing to imaging. Eleventh, always document baseline testosterone, LH, FSH, and prolactin before any intervention to gauge response. Twelfth, educate the patient that monitoring hematocrit and PSA is still essential if they later start TRT, even after correcting the underlying cause. Thirteenth, a multidisciplinary approach involving endocrinology, radiology, and sometimes neurosurgery yields the best outcomes. Fourteenth, keep in mind that pituitary function can be dynamic; repeat labs after a few months may reveal a trend that a single snapshot misses. Finally, clear communication about the rationale for each test helps patients stay engaged and reduces anxiety about “too many scans”.
Franco WR November 18, 2025 AT 10:27
When the root cause is reversible-like cutting back on chronic opioid use or addressing uncontrolled diabetes-the hormonal axis can bounce back on its own. In my clinic we’ve seen men regain normal testosterone levels after just 6‑8 weeks of lifestyle overhaul without any exogenous hormones. It’s a powerful reminder that the body often knows how to recalibrate when you remove the blockages.
Rachelle Dodge November 25, 2025 AT 09:07
The pituitary’s like a dimmer switch; turn it up gently with SERMs and you’ll avoid the glare of full‑blown TRT.
Gaurav Joshi December 2, 2025 AT 07:47
Addressing metabolic syndrome simultaneously with hormone therapy boosts the efficacy of TRT by reducing aromatase activity, which otherwise converts testosterone to estrogen and dampens the feedback loop.
Elaine Proffitt December 9, 2025 AT 06:27
Regular monitoring of hematocrit every three months prevents polycythemia, a hidden danger of testosterone therapy that can lead to serious clotting events if ignored.
Christopher Munt December 16, 2025 AT 05:07
Strength training spikes natural testosterone.
Sangeeta Birdi December 23, 2025 AT 03:47
Remember, sleep isn’t optional – deep REM cycles are when the body naturally pumps out the most testosterone 🌙. Prioritize 7‑9 hours and you’ll likely see a noticeable lift in energy.
Chelsea Caterer December 30, 2025 AT 02:27
Dont forget to check PSA yearly when on TRT it safe to keep an eye on prostate health.
Lauren Carlton January 6, 2026 AT 01:07
The article contains several punctuation errors; for example, the list items lack consistent Oxford commas, and the phrase “low testosterone even though the testes themselves are fine” should be set off with commas for clarity.
Katelyn Johnson January 12, 2026 AT 23:47
Building a support network-whether it’s a fitness group, a nutritionist, or an online forum-can provide accountability and emotional encouragement during the hormone recovery journey.
Patrick Fortunato January 19, 2026 AT 22:27
Irish lads don’t need a pill to feel robust; a proper diet, cold‑water swims, and hard work on the farm keep the hormones humming naturally.
Write a comment