People taking atorvastatin for high cholesterol sometimes notice new symptoms-dry eyes, a gritty feeling in the mouth, or persistent fatigue. If they’ve heard of Sjögren’s Syndrome, it’s natural to wonder: is this drug causing it? Or is it just coincidence? The truth isn’t simple, but it’s not scary either. There’s no clear proof that atorvastatin causes Sjögren’s Syndrome. But there are enough odd reports and biological clues to make doctors pay attention.
What is Sjögren’s Syndrome?
Sjögren’s Syndrome is an autoimmune disorder where the body’s immune system attacks its own moisture-producing glands. That means the tear ducts and salivary glands get damaged, leading to the classic signs: dry eyes and dry mouth. But it doesn’t stop there. Many people with Sjögren’s also experience joint pain, fatigue, brain fog, and even nerve damage. It’s not rare-about 4 million people in the U.S. have it, mostly women over 40. The average diagnosis takes seven years because symptoms creep in slowly and look like other conditions.
The root cause? No one knows for sure. Genetics play a role, and viruses like Epstein-Barr might trigger it in susceptible people. But drugs? That’s a newer area of study.
What is Atorvastatin?
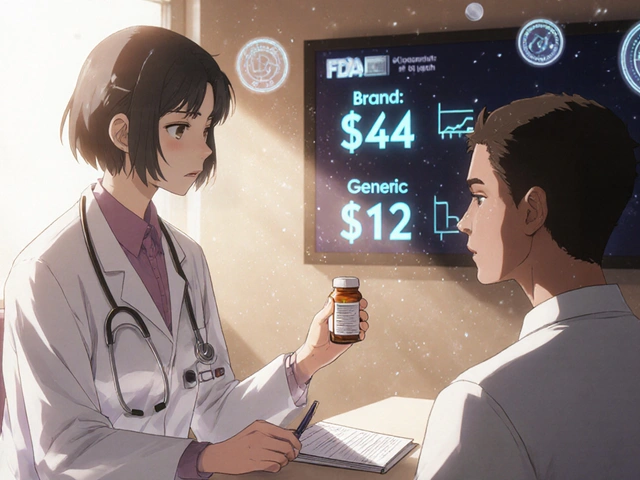
Atorvastatin is one of the most prescribed statins in the world. It lowers LDL (bad) cholesterol by blocking an enzyme in the liver called HMG-CoA reductase. It’s sold under brand names like Lipitor and is available as a generic. Millions take it daily to reduce heart attack and stroke risk. Side effects? Muscle pain, liver enzyme changes, and in rare cases, diabetes. But autoimmune disease? That’s not listed on the label.
Still, statins don’t just lower cholesterol. They also have anti-inflammatory effects. That’s why researchers started looking at whether they might help-or hurt-autoimmune conditions like rheumatoid arthritis or lupus. Sjögren’s? That’s less studied.
Could Atorvastatin Trigger Sjögren’s?
There’s no large-scale study proving atorvastatin causes Sjögren’s Syndrome. But case reports exist. In 2019, a team in Italy published a case of a 62-year-old woman who developed severe dry eyes and mouth six months after starting atorvastatin. Her anti-SSA and anti-SSB antibodies-key markers for Sjögren’s-came back positive. When she stopped the drug, her symptoms improved. When she restarted it, they came back. That’s a classic drug-induced flare pattern.
Another case in 2021 involved a 58-year-old man in Japan. He’d been on atorvastatin for three years. Then he developed swollen salivary glands, dry mouth, and difficulty swallowing. A biopsy confirmed lymphocytic infiltration of his salivary glands-the hallmark of Sjögren’s. He had no prior autoimmune history. After stopping atorvastatin, his symptoms resolved within three months.
These aren’t flukes. They’re rare, but they’re consistent. The timing matches. The immune markers align. And when the drug is removed, things get better.
How Could a Cholesterol Drug Cause an Autoimmune Reaction?
Statins like atorvastatin don’t just lower cholesterol. They affect immune cells too. Studies show they can reduce levels of inflammatory proteins like TNF-alpha and IL-6. That sounds good-until you realize that in some people, the immune system needs a little inflammation to stay balanced.
One theory is that atorvastatin alters how immune cells present antigens. In genetically prone individuals, this might confuse the immune system into mistaking glandular tissue for a threat. Another idea: statins can change the structure of cell membranes. If your salivary gland cells start looking “foreign” to your immune system, it might attack them.
There’s also a link between statins and increased levels of certain autoantibodies. A 2020 analysis in the Journal of Autoimmunity found that statin users had slightly higher rates of anti-SSA antibodies-even without symptoms. That doesn’t mean Sjögren’s, but it suggests the immune system is being nudged in a direction that could, in rare cases, tip into full-blown disease.
Who’s at Risk?
If you’re on atorvastatin and start noticing dry eyes, dry mouth, or a persistent scratchy throat, don’t panic. But do pay attention. Risk factors include:
- Being female (Sjögren’s affects women 9 times more than men)
- Age over 50
- Having another autoimmune condition (like thyroid disease or rheumatoid arthritis)
- Genetic markers like HLA-DR3 or HLA-DR5
- Long-term statin use (over 2 years)
It’s not about the dose. Even low-dose atorvastatin (10 mg) has been linked to cases. It’s about individual biology.
What Should You Do?
If you’re on atorvastatin and have new dryness symptoms:
- Don’t stop the drug on your own. Cholesterol control matters for heart health.
- See your doctor. Mention the timing-when you started the drug and when symptoms began.
- Ask for a Schirmer’s test (measures tear production) and a salivary flow test.
- Request blood tests for anti-SSA and anti-SSB antibodies.
- If tests are positive, your doctor might consider switching you to a different cholesterol medication.
There are alternatives. Rosuvastatin, pravastatin, and ezetimibe don’t have the same case reports. Some doctors prefer pravastatin for patients with autoimmune concerns because it’s less likely to cross cell membranes and affect immune cells.
Is Atorvastatin Safe for People With Sjögren’s?
If you already have Sjögren’s Syndrome, there’s no evidence that atorvastatin makes it worse. In fact, some small studies suggest statins might help reduce inflammation in autoimmune diseases. A 2023 pilot study in patients with Sjögren’s and high cholesterol found no increase in dryness symptoms after six months on atorvastatin. Some even reported less joint pain.
So if you have Sjögren’s and need to lower your cholesterol, atorvastatin is probably fine. But if you’re developing symptoms for the first time while on it? That’s different.
What the Experts Say
The American College of Rheumatology doesn’t list statins as a known trigger for Sjögren’s. But they do say: "Drug-induced autoimmune phenomena are underrecognized." The European League Against Rheumatism (EULAR) has called for more research into statin-autoimmune links.
Dr. Helen Liu, a rheumatologist at Mayo Clinic, told Arthritis Today in 2024: "We see maybe one or two cases a year where a patient’s dryness symptoms clearly started after a statin. It’s rare, but when it happens, it’s unmistakable. We don’t blame the drug, but we don’t ignore it either. It’s a signal to look deeper."
The Bottom Line
Atorvastatin doesn’t cause Sjögren’s Syndrome in most people. For the vast majority, it’s a safe, life-saving drug. But in a small number of genetically sensitive individuals, it may act as a trigger. The symptoms-dry eyes, dry mouth, fatigue-are real. And they can be reversed if caught early.
If you’re taking atorvastatin and notice persistent dryness, don’t assume it’s aging or screen time. Talk to your doctor. Get tested. Your immune system might be trying to tell you something.
And if you’re already diagnosed with Sjögren’s? Atorvastatin is likely still safe. But keep an eye on your symptoms. Change in dryness? Report it. Your care team needs to know.
Frequently Asked Questions
Can atorvastatin cause dry eyes and dry mouth?
Yes, in rare cases. While not a common side effect, there are documented cases where people developed dry eyes and dry mouth after starting atorvastatin. These symptoms often matched the clinical signs of Sjögren’s Syndrome. In some patients, stopping the drug led to symptom improvement. This suggests a possible link in susceptible individuals, though it’s not a typical reaction.
Is Sjögren’s Syndrome caused by statins?
No, statins like atorvastatin do not cause Sjögren’s Syndrome in the general population. Sjögren’s is an autoimmune disease triggered by a mix of genetics and environmental factors. However, in rare cases, statins may act as a trigger in people who are already genetically predisposed. These are not cases of the drug causing the disease outright, but possibly accelerating its onset in vulnerable individuals.
What should I do if I think atorvastatin is causing my dryness symptoms?
Don’t stop taking it without talking to your doctor. Instead, schedule an appointment and describe when your symptoms started relative to when you began the medication. Ask for tests for anti-SSA and anti-SSB antibodies, a Schirmer’s test for tear production, and a salivary flow test. If results suggest Sjögren’s, your doctor may consider switching to another cholesterol-lowering drug like pravastatin or ezetimibe.
Are there safer statins for people with autoimmune concerns?
Pravastatin and rosuvastatin are often preferred in patients with autoimmune conditions because they’re less likely to penetrate cell membranes and affect immune function. Atorvastatin and simvastatin cross membranes more easily, which may explain why they’re more often linked to rare autoimmune reactions. But the difference is small, and individual response varies. Always discuss options with your doctor.
Can I take atorvastatin if I already have Sjögren’s Syndrome?
Yes, most people with Sjögren’s can safely take atorvastatin. There’s no strong evidence that it worsens the condition. In fact, some studies suggest statins may help reduce inflammation in autoimmune diseases. However, if you notice your dryness symptoms suddenly get worse after starting the drug, tell your doctor. It could be unrelated, or it could be a sign you need a different medication.






Posts Comments
Michael Petesch November 18, 2025 AT 21:43
Interesting breakdown. I’ve been on atorvastatin for five years and noticed my eyes felt grittier last winter, but I attributed it to indoor heating. The case reports you cited are compelling-especially the reversibility upon discontinuation. This deserves more attention in primary care guidelines.
Reema Al-Zaheri November 20, 2025 AT 19:03
While the biological plausibility is intriguing, correlation does not imply causation. The absence of large-scale epidemiological data means we cannot conclude that atorvastatin triggers Sjögren’s Syndrome. The cases cited are anecdotal, and confounding variables-such as age, hormonal shifts, or concurrent medications-are not adequately controlled. Caution is warranted, but alarm is premature.
Michael Salmon November 22, 2025 AT 03:09
Oh great. Another ‘statins are secretly destroying your immune system’ scare piece. You cite two case reports and call it evidence? Millions take this drug daily. If it were triggering autoimmune disease at any meaningful rate, we’d see it in pharmacovigilance databases. We don’t. Stop fearmongering with cherry-picked anecdotes.
Joe Durham November 23, 2025 AT 04:53
Both sides have a point. The contrarian view is right that this is rare-but the original post is right that rare doesn’t mean irrelevant. If someone’s dry eyes started right after starting a new med, and they have HLA-DR3, it’s worth investigating. No need to panic, but no need to dismiss either. Medicine is about nuance, not absolutes.
Derron Vanderpoel November 24, 2025 AT 01:49
I started atorvastatin in 2021 and by 2022 I could barely swallow my morning coffee-felt like sandpaper in my throat. I thought I was dying. Went to a rheumatologist, got the antibodies, diagnosed with Sjögren’s. Stopped the drug. Within 8 weeks, my mouth felt human again. I’m not a doctor, but I’m living proof this can happen. Don’t ignore your body.
Timothy Reed November 24, 2025 AT 15:51
Well-structured and balanced. The key takeaway is awareness, not avoidance. For patients with high cardiovascular risk, the benefits of atorvastatin far outweigh the theoretical autoimmune risk. But for those with new-onset sicca symptoms and genetic susceptibility, a medication switch may be prudent. Shared decision-making is essential here.
harenee hanapi November 25, 2025 AT 21:00
Oh wow, so now statins are the new villains? I’ve had Sjögren’s for 12 years and my doctor says it’s from my mom’s side of the family, not some pill. Why do people always blame drugs? You’re all just looking for someone to blame instead of accepting that your body is just… broken. Sad.
Christopher Robinson November 26, 2025 AT 13:12
👏 Great post. I’m a pharmacist and I’ve seen this exact scenario 3x in the last 2 years. Two women, mid-50s, on atorvastatin for 3+ years, developed dry eyes + parotid swelling. Both had anti-SSA+. Both improved after switching to pravastatin. No one else noticed because no one asked. Always ask about timing.
James Ó Nuanáin November 27, 2025 AT 14:22
It is lamentable that the British National Health Service continues to prescribe atorvastatin as a first-line agent without adequate screening for autoimmune predisposition. In the United Kingdom, we have a long-standing tradition of medical prudence-yet here we are, allowing pharmaceutical convenience to override clinical caution. This is not innovation; it is negligence.
Nick Lesieur November 28, 2025 AT 06:34
lol so you’re telling me my dry mouth is from Lipitor? Maybe it’s from drinking 12 coffees a day and never drinking water? Just a thought. Also, ‘anti-SSA’? That’s not even a real thing, right? Sounds like a lab report from a sci-fi movie. 😂
seamus moginie November 29, 2025 AT 12:17
Enough with the ‘it’s just coincidence’ nonsense. My sister’s case was identical-started atorvastatin, dry eyes within months, antibodies positive, symptoms vanished after switching meds. You can’t dismiss this as ‘anecdotal’ when it’s happening across continents with the same pattern. This isn’t fear-it’s observation. And if you’re a doctor who ignores this, you’re failing your patients.
Write a comment