You walk into the doctor’s office, and you can already sense it: another conversation about why this keeps happening. Recurrent miscarriages, sometimes called 'repeated pregnancy loss,' aren’t just statistics—they ripple through every part of a woman’s life, from her sense of self to her relationships with others. If you’re reading this because you or someone close to you is facing miscarriage after miscarriage, you’re not alone. Research actually shows around 1 in 50 women experience three or more consecutive losses—way more common than most realize. Many women never find a straightforward answer to why this is happening. But lately, there’s been growing attention on a hormone therapy called dydrogesterone, and for good reason: it may offer an important step forward for those who feel like they’ve exhausted every option.
Understanding Recurrent Miscarriages: Why Does This Happen?
Talk about feeling powerless—recurrent miscarriage, usually defined as losing two or three pregnancies in a row before 20 weeks, is a medical situation that tests a woman both physically and emotionally. While doctors might tell you about all the potential reasons—genetic issues, immune problems, thyroid levels, even lifestyle factors—the tough reality for a lot of women is that many cases end up in the category “unexplained.”
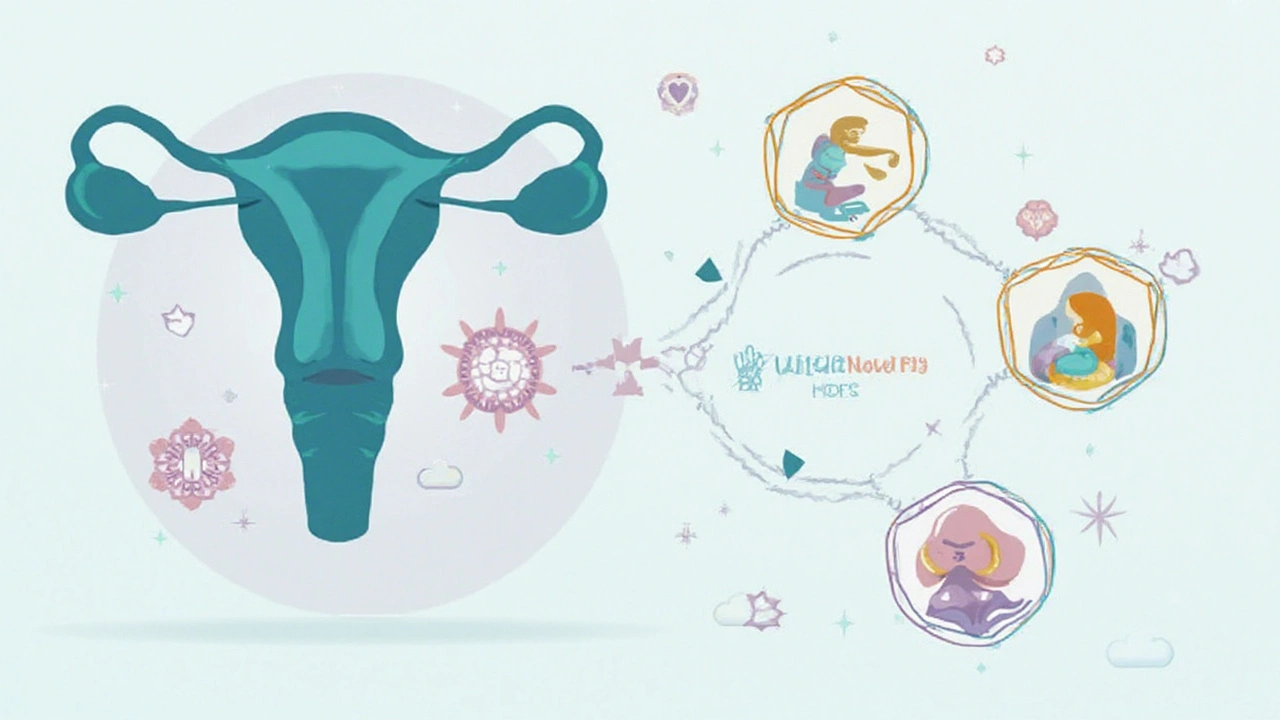
Let’s break it down a bit. Around 50% of couples experiencing recurrent miscarriage never find a specific cause, especially after all the standard tests (think chromosome analysis, blood clotting screens, and uterine scans). Some research points to the lining of the uterus not being receptive enough, or maybe a problem with hormone levels. The star hormone in early pregnancy is progesterone—sometimes called the “pregnancy hormone.” Not only does it prep your uterus to welcome an embryo, but it also calms the uterine muscles so they’re less likely to contract early. If your body can’t produce enough progesterone, or if the timing is off, the odds of a healthy pregnancy can take a big hit. But even women with supposedly 'normal' hormone tests have seen improvement with progesterone support.
Don’t buy into the idea that recurrent miscarriages “just happen” or, worse, that it’s somehow your fault. There are many ways women seek answers: specialized blood work, detailed ultrasounds, hysteroscopies, or even tracking ovulation with apps and basal body temperature thermometers. Tackling lifestyle factors—like quitting smoking, lowering stress, or avoiding certain medications—can also nudge the odds in your favor. But, for many women, hormone therapy is where things really start to shift. Enter dydrogesterone—an option that’s gaining traction around the world.
Just to give you a snapshot, here’s a recent overview of causes of recurrent miscarriage and how often they show up in clinical studies:
| Cause | Approximate Frequency (%) |
|---|---|
| Genetic (chromosome errors) | 2-5 |
| Anatomical (uterine abnormalities) | 10-15 |
| Endocrine (hormonal issues) | 15-20 |
| Immune (autoimmune or alloimmune) | 10-20 |
| Unexplained | 45-50 |
Notice how the biggest slice belongs to unexplained losses? That’s where treating with progesterone analogues, like dydrogesterone, gets really interesting. It may offer benefits even when the cause remains a mystery.

Dydrogesterone Therapy: What Is It and How Does It Work?
If you’ve heard of progesterone therapy, you’re probably wondering what makes dydrogesterone special. This medication isn’t new—it’s actually been available since the 1960s—but recent studies have thrown it back into the spotlight for miscarriage management. Dydrogesterone is a synthetic form of progesterone, but unlike some older versions, it’s designed to closely mimic your body’s natural hormone, with fewer side effects.
Here’s how dydrogesterone stands out:
- It’s taken by mouth (orally), so you don’t have to deal with injections or messy vaginal gels.
- It doesn’t cause the bloating, drowsiness, or “overheating” that women sometimes feel with other forms of progesterone.
- It’s highly targeted, meaning it does its job in the uterus without acting on other hormone systems (like androgens or corticosteroids).
What does dydrogesterone actually do in early pregnancy? It helps stabilize the lining of the uterus, promotes implantation, and supports the immune system in keeping the embryo “safe” from rejection. A major multicenter study published in The New England Journal of Medicine in 2022 looked at over 1,400 women with a history of recurrent miscarriage. They gave half of the women dydrogesterone and the other half a placebo. At 20 weeks, 68% of the women using dydrogesterone were still pregnant versus 60% in the placebo group. That may sound like a modest jump, but in the world of recurrent pregnancy loss, it’s a massive difference. For many women, it means finally carrying a pregnancy beyond the danger zone.
A few facts women are often curious about:
- Dydrogesterone is usually started shortly after confirming pregnancy and continued to at least 20 weeks, sometimes longer.
- Doses vary, but commonly prescribed doses are 10-30 mg daily (always follow your doctor’s plan).
- It’s considered well-tolerated, with side effects mainly being mild (like headache, breast tenderness, or mild spotting).
- There’s no reliable evidence that dydrogesterone increases the risk of birth defects or long-term problems in babies—this has been a concern with some older hormones, but newer safety data are reassuring.
If you’re thinking, “Why have I never heard of this?”—well, progesterone supplements are more popular in Europe, the Middle East, and Asia than in the U.S. That’s slowly changing as newer research supports its use.
Check out these results from a real-world clinical study:
| Treatment Group | Ongoing Pregnancy Rate (%) | Live Birth Rate (%) |
|---|---|---|
| Placebo | 61 | 57 |
| Dydrogesterone | 70 | 67 |
For those who have been through round after round of heartache, this is hope on a page. And for many women, dydrogesterone therapy is part of a bigger “toolkit” that might include other meds, lifestyle changes, and thorough medical workups.
Practical Tips and What to Expect: Making Dydrogesterone Therapy Work for You
Stepping into progesterone therapy can feel like new territory, but women who succeed with it often share some habits in common. First, don’t wait to talk to your doctor—if you’ve had two or more early losses, early intervention boosts your odds. Ask whether your doctor is familiar with dydrogesterone, and if it isn’t available locally, find out if alternative forms or branded names exist in your area (like Duphaston).
One big tip: tracking matters. Women who keep a journal or use a pregnancy tracking app report feeling more in control, which actually helps manage anxiety levels. Write down when you take your meds, how you feel, and any symptoms, even small ones. If you experience minor spotting or cramping, don’t panic—let your doctor know, but keep taking your medication unless told otherwise. Missing doses isn’t the end of the world, but try to keep it on a schedule to keep hormone levels steady. Many women set a phone reminder or tie it in with another daily habit, like brushing their teeth.
Here’s a checklist for navigating dydrogesterone therapy:
- Before starting: Gather your history—write down dates of previous miscarriages, any testing results, and any symptoms (spotting, pain, etc.).
- During therapy: Take your tablets at the same time each day. Keep up with routine blood tests and ultrasound appointments. Stay well-hydrated and rested.
- If side effects pop up: Mild headaches or breast pain are the most common. These usually improve with time. If you have severe symptoms, catch your doctor right away.
- Emotional care: Miscarriage takes a toll on your mental health. Consider joining a support group (online or locally), or talking with a counselor familiar with pregnancy loss. Many women say sharing with others turns guilt or isolation into strength.
- Lifestyle: Gentle exercise, stress management (like meditation or yoga), eating a variety of healthy foods, and avoiding alcohol/smoking—these are not magic solutions, but they work synergistically with the medication to support your body.
- Family/friends: Let those closest to you know what you’re going through, if you’re comfortable. Support makes a massive difference, even if it just means someone to listen on a tough day.
One myth that’s worth busting: progesterone, including dydrogesterone, isn’t just “extra padding.” It acts in precise, science-backed ways. And even if you’ve heard “there’s no guarantee,” many women who use it after recurrent miscarriages see their first-ever positive outcome. That can change everything—not just for the current pregnancy, but also for emotional healing after loss.
If you’re nervous about side effects or drug interactions, bring a list of all the supplements or medications you use to your doctor’s visit. Dydrogesterone can technically interact with certain epilepsy meds or some antibiotics, but for most women, the interaction risk is low. You don’t need to overthink your diet either—just eat what feels nourishing and avoid food-borne illness risks (like unpasteurized cheeses or undercooked eggs), exactly as you would in any pregnancy.
And one last fact to keep in mind: a 2023 review looking at over 20,000 pregnancies around the world found no higher risk of birth defects or childhood cancer with dydrogesterone compared to pregnancies without it. If you’re someone who combs through online forums late at night, searching for reassurance, remember that scary anecdotes don’t equal real, large-scale data. Scientific reviews remain the gold standard.
You don’t have to give up or accept endless cycles of heartbreak as your fate. Sometimes, one small addition to your treatment plan—something as deceptively simple as a hormone tablet—can tilt the odds in your favor for the first time in years. Keep asking questions, keep tracking your symptoms, and don’t lose hope: dydrogesterone therapy could be the piece you’ve been missing in managing recurrent miscarriages.







Posts Comments
Cecily Bogsprocket June 12, 2025 AT 05:29
It’s funny how we’re told to trust science, but then when something like dydrogesterone shows up-something that’s been used safely for decades overseas-it’s treated like fringe medicine. I lost three pregnancies before I even got to the point of asking about progesterone. My doctor shrugged and said, ‘Maybe it’s just bad luck.’ I spent months reading studies, talking to women on forums, and finally found a reproductive endocrinologist who actually listened. Dydrogesterone wasn’t magic, but it was the first thing that made me feel like my body wasn’t broken-it was just missing a piece. Now I’m 28 weeks along. I don’t know if it was this, or the therapy, or just time, but I’m holding onto hope again.
Emma louise June 12, 2025 AT 16:05
Oh great, another ‘natural progesterone’ scam dressed up in lab coats. Next they’ll be selling us moon dust and unicorn tears for fertility. The FDA hasn’t approved this for miscarriage prevention in the US for a reason. You think your 8% higher live birth rate is ‘hope’? That’s a p-value whisper. Stop letting Big Pharma sell you false comfort while they charge $200 a month for a pill that’s basically just a placebo with extra steps.
Miriam Lohrum June 12, 2025 AT 16:12
It’s interesting how the medical community treats unexplained recurrent loss as a black box, then reaches for hormonal fixes without fully understanding the mechanism. Dydrogesterone may work, but why? Is it immune modulation? Endometrial receptivity? Or just a placebo effect amplified by hope? The data is promising, but the lack of mechanistic clarity leaves me uneasy. We’ve been here before-with heparin, with intralipids, with IVIG. All had small effect sizes. We need better biomarkers, not just more pills.
Emma Dovener June 12, 2025 AT 23:22
In India, dydrogesterone has been used for decades under the brand Duphaston. My aunt took it after three losses and carried two healthy babies to term. It’s not a cure-all, but it’s one of the few interventions with consistent data across cultures. The resistance in the U.S. feels more like institutional inertia than scientific skepticism. Doctors here are trained to wait for FDA approval before considering anything, even if it’s been standard care elsewhere for 40 years. We need to catch up.
Rhiana Grob June 13, 2025 AT 06:37
I appreciate the depth of this post. For anyone navigating recurrent loss, I want to say: your grief is valid, your persistence is brave, and your body is not failing you. Dydrogesterone isn’t a miracle, but it’s one of the few tools with real data behind it. If your provider dismisses it, find someone who won’t. You deserve care that sees you as more than a statistic. And if you’re reading this and feeling alone-reach out. There are thousands of us out here, holding space for each other.
Rebecca Price June 15, 2025 AT 05:45
Look, I get why people are skeptical. But let’s be real: when you’ve lost three pregnancies, you’ll try anything that doesn’t involve surgery or experimental gene therapy. Dydrogesterone is cheap, safe, and oral-no needles, no mess. My OB didn’t even bring it up until I asked. She said, ‘It’s not standard here.’ I said, ‘Then why is it standard everywhere else?’ She looked it up that night and prescribed it the next day. I’m 22 weeks now. I don’t care if it’s placebo or science-I’m alive, and so is my baby. That’s enough.
shawn monroe June 15, 2025 AT 10:05
OMG. I JUST FOUND OUT I’M 8 WEEKS WITH DYDROGESTERONE AND I’M CRYING RIGHT NOW 😭😭😭 I lost two before this. My doc said ‘it’s probably chromosomal’ and I was ready to give up. Then I found this thread. Started dydrogesterone at 5 weeks. No spotting. No panic. Just… quiet hope. I’m not saying it’s magic. But if this works? I’m gonna buy every bottle in the pharmacy. THANK YOU FOR WRITING THIS. 🙏
marie HUREL June 16, 2025 AT 21:18
I’m not sure if this helped me, but it didn’t hurt. I took it after my second loss, just to feel like I was doing something. I didn’t get pregnant again until the third try-and I didn’t take it then. So maybe it was the timing. Or maybe it was just luck. Either way, I’m glad I tried it. I don’t regret it. And I’m glad others are finding hope in it too.
Edward Batchelder June 18, 2025 AT 18:52
Let me be clear: recurrent miscarriage is not a failure of willpower, not a punishment, not a sign of weakness. It is a biological phenomenon, often rooted in complex endocrine and immunological pathways that modern medicine is only beginning to map. Dydrogesterone, as a selective progesterone receptor modulator, offers targeted support to the endometrial microenvironment without systemic hormonal disruption. The 70% ongoing pregnancy rate in the NEJM study is not merely statistically significant-it is profoundly human. You are not broken. You are not alone. And you are not beyond help.
Gayle Jenkins June 20, 2025 AT 13:11
If your doctor doesn’t know what dydrogesterone is, fire them. Seriously. This isn’t 1998. You’ve got studies, you’ve got global usage, you’ve got safety data. If they’re still stuck in ‘unexplained = no treatment’ mode, they’re not your ally. I asked for it after my second loss. Got laughed at. Went to a REI. Got it. Got pregnant. Got a baby. Done. Stop waiting for permission to fight for your body.
Allison Turner June 22, 2025 AT 03:15
So let me get this straight. You’re saying a $200/month pill that’s not even FDA-approved for this use is the answer? What’s next, acupuncture and crystals? I’ve seen this movie before. Every year it’s a new ‘miracle cure’ for miscarriage. None of them work long-term. You’re just giving people false hope so they’ll keep paying for more tests, more pills, more desperation.
Darrel Smith June 23, 2025 AT 16:35
People need to stop acting like this is some kind of miracle. Progesterone has been around forever. It’s not new. It’s not special. It’s just a hormone. And if your body can’t make enough of it, maybe you shouldn’t be pregnant. Maybe your body is telling you something. I’ve seen too many women chase pills instead of facing the truth: sometimes, nature knows better than we do.
Aishwarya Sivaraj June 25, 2025 AT 09:21
i read this in india where we use duphaston since 1980s and it saved many lives i lost 2 babies then took it at 5 weeks and now my daughter is 3 years old. no side effects just a small headache at first but went away. please dont ignore this just because usa not use it. science dont have borders. love from india 🇮🇳
steve stofelano, jr. June 25, 2025 AT 17:22
It is my considered opinion, based upon a thorough review of the peer-reviewed literature and clinical guidelines issued by the European Society of Human Reproduction and Embryology, that dydrogesterone represents a paradigmatic advancement in the management of unexplained recurrent pregnancy loss. Its pharmacokinetic profile, combined with its receptor specificity and low incidence of adverse effects, renders it a superior alternative to micronized progesterone in oral form. The data presented in the 2022 NEJM trial are not merely suggestive-they are compelling. I urge clinicians to integrate this agent into standard protocols without delay.
Sam HardcastleJIV June 26, 2025 AT 13:04
One might be tempted to view this as a triumph of medical science. But one must also ask: why is it that women are expected to swallow synthetic hormones to compensate for a system that, by design, is meant to fail? Is it not more honest to acknowledge that our bodies are not machines to be fixed, but complex ecosystems that may, at times, choose not to sustain? Dydrogesterone may prolong pregnancy-but does it address the deeper question of why pregnancy fails in the first place?
Mira Adam June 28, 2025 AT 03:01
It’s not about the pill. It’s about how we’ve been trained to believe that if we just take enough pills, we can outsmart nature. You think dydrogesterone is the answer? Then why do 30% still lose? Why is it only 70%? Maybe the real problem isn’t progesterone-it’s the assumption that every loss can be fixed. Some things aren’t meant to be controlled.
archana das June 29, 2025 AT 16:21
i am from india and i saw my sister take this after 3 losses and now she has 2 kids. it is not magic but it is kind. in our culture we dont talk about loss but this medicine gave us quiet hope. i wish more women knew. thank you for writing this
Sue Haskett June 30, 2025 AT 13:44
PLEASE-don’t wait for your doctor to bring it up. Ask for dydrogesterone. Write down your loss dates. Bring this article. Print the NEJM study. You are your own best advocate. I waited 18 months after my second loss to ask. Don’t make that mistake. I’m 24 weeks now. I owe this to myself for not giving up. You deserve this chance too.
Write a comment