When a product leaves a manufacturing facility, it should be safe. Not just safe by chance - safe because every step was controlled. That’s where environmental monitoring comes in. It’s not about checking the final product. It’s about asking: Is the environment where the product is made clean enough? In pharmaceuticals, food processing, and cosmetics, contamination doesn’t always come from raw materials. Sometimes, it comes from the floor, the air, the drain, or even a poorly cleaned conveyor belt. Environmental monitoring is the system that catches those hidden risks before they ruin a batch - or worse, hurt a consumer.
Why Environmental Monitoring Isn’t Optional
Think of a pharmaceutical cleanroom. Every surface, every breath of air, every drop of water is part of the equation. A single fungal spore landing on a vial during filling can turn a life-saving drug into a hazard. The FDA doesn’t just recommend monitoring - it requires it. The same goes for ready-to-eat food facilities. Listeria monocytogenes doesn’t care if your factory is small or large. If it’s in your Zone 1 surface - the slicer, the conveyor, the packaging line - it can contaminate thousands of products before anyone notices. The numbers tell the story. According to the USDA, foodborne illnesses tied to environmental contamination cost the U.S. economy $77.7 billion in 2022. The CDC found that 87% of those outbreaks could have been prevented with proper environmental sampling. That’s not a statistic - that’s a failure of process. Facilities that skip or cut corners on environmental monitoring aren’t saving money. They’re gambling with recalls, lawsuits, and lives.The Zone System: Your Blueprint for Risk
You can’t monitor everything. So you focus on what matters. That’s where the zone classification system comes in. It’s not just industry jargon - it’s a practical risk map.- Zone 1: Direct food or drug contact surfaces. Think slicers, mixers, filling nozzles, packaging rollers. These are sampled daily or even after every shift. A single swab here can prevent a recall.
- Zone 2: Surfaces near Zone 1 - equipment housings, refrigeration units, nearby carts. These are sampled weekly. Condensation dripping from an overhead pipe? That’s a Zone 2 risk.
- Zone 3: Remote but still in the production area - forklifts, tool racks, maintenance carts. You might think these are low risk. But a PPD Laboratories study found that 62% of all contamination events traced back to Zone 3 and 4 surfaces. Floors. Drain covers. Door handles. These are silent vectors.
- Zone 4: Outside the production area - break rooms, hallways, storage. Monitored monthly. Still important. A worker tracking in dirt from the parking lot can carry pathogens into Zone 3.
How Testing Works: From Swabs to Sequences
Sampling isn’t just wiping a surface and sending it off. It’s science. For microbiological testing, sterile sponges or swabs collect samples from surfaces. Air is pulled through liquid impingers or solid impactors - devices that capture airborne particles and microbes. The results? Colony-forming units per cubic meter (CFU/m³). That number tells you if your air is clean enough for an ISO Class 5 cleanroom (pharma) or if your food line is at risk for Listeria. Water systems are checked differently. Pharmaceutical facilities use total organic carbon (TOC) and conductivity tests to meet USP <645> standards. Food plants focus on EPA-regulated municipal water safety. Metals? That’s ICP (inductively coupled plasma) testing. Chemical residues? HPLC or GC-MS. Each contaminant needs its own tool. And then there’s ATP testing. It’s not a replacement for microbiological tests, but it’s a game-changer for speed. ATP detects organic residue - sweat, grease, food particles - that could feed bacteria. Results come in seconds. FDA data shows facilities using ATP see 32% faster turnaround between production runs. Why? Because you don’t wait 48 hours to know if a surface is clean. You know in 10 seconds. That means less downtime, less waste, and more control.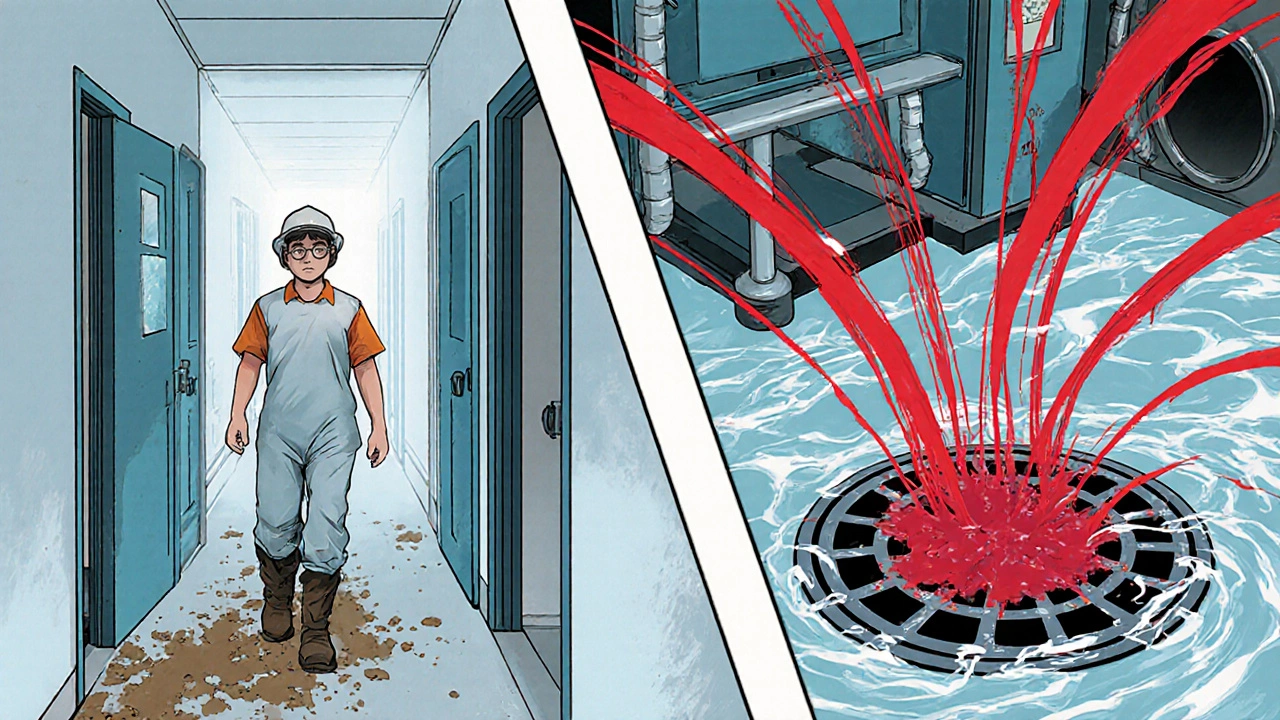
What the Regulators Really Want
The FDA, EMA, and USDA don’t want checklists. They want proof of control. In pharmaceuticals, EU GMP Annex 1 (updated August 2023) demands real-time monitoring of temperature, humidity, and particulates in critical areas. You can’t just test once a week. You need trending. You need alarms. You need data that shows your environment is stable - not just clean on the day of inspection. For food, the USDA’s Listeria Rule (9 CFR Part 430) is brutal. If you make ready-to-eat products - deli meats, salads, smoked fish - you must test Zone 1 surfaces for Listeria at least weekly. And you must document every positive result, every corrective action, every retest. Miss one, and your facility gets flagged. Repeat it, and you’re on the FDA’s watchlist. The bottom line? Regulators aren’t looking for perfection. They’re looking for consistency. They want to see that you know where your risks are, that you test them regularly, and that you fix problems before they become outbreaks.Common Pitfalls - And How to Avoid Them
Even well-intentioned facilities fail. Here’s what goes wrong - and how to fix it.- Inconsistent sampling technique: 68% of facilities struggle with this. Swabbing too lightly. Not sterilizing samplers. Using the same swab for multiple zones. Training isn’t optional. FDA recommends 40 hours of hands-on practice before staff can collect official samples.
- Poor data integration: ATP results, microbiological results, allergen tests, and chemical data often sit in separate systems. No one connects the dots. If a surface tests high for ATP and then later tests positive for Salmonella, that’s not a coincidence. It’s a pattern. You need software that ties it all together.
- Over-reliance on one method: Some facilities think ATP = clean. It doesn’t. It only shows organic residue. You still need microbiological tests to catch pathogens. Others skip air sampling because it’s expensive. Bad move. Airborne contamination is silent and deadly.
- Ignoring Zone 3 and 4: As the PPD study showed, most contamination events come from surfaces people think are low risk. Floors. Drain covers. Door handles. Train your team to treat these areas with the same seriousness as Zone 1.

The Future: AI, Sequencing, and Real-Time Control
Environmental monitoring is evolving fast. Next-generation sequencing (NGS) is replacing old-school culturing. Instead of waiting 72 hours to identify a mold, you can now sequence its DNA in under 24 hours. That means faster root cause analysis. Faster recalls. Fewer lost batches. AI is coming in too. By analyzing years of environmental data - temperature spikes, humidity changes, swab results - machine learning can predict where contamination is likely to occur. One manufacturer in Germany reduced false positives by 27% by linking environmental monitoring data with culture contamination logs. That’s not magic. That’s smart data use. By 2027, 38% of environmental monitoring systems will use AI-driven analytics, up from just 12% in 2022. The market is growing - from $7.2 billion in 2022 to $12.5 billion by 2027. Why? Because companies are realizing: Contamination control isn’t a cost. It’s a competitive advantage.Where to Start
If your facility doesn’t have a solid environmental monitoring program, don’t panic. Start here:- Map your zones. Walk every square foot. Label every surface. Get input from production, maintenance, and quality.
- Define your sampling frequency. Zone 1: daily or after each shift. Zone 2: weekly. Zone 3: monthly. Zone 4: quarterly. Adjust based on your risk.
- Train your team. No exceptions. Use sterile technique. Document every step.
- Start with ATP for quick feedback. Add microbiological testing for confirmation.
- Invest in data software. Don’t let results sit in spreadsheets. Connect them. Trend them. Alert on anomalies.
Final Thought
Environmental monitoring isn’t about passing an audit. It’s about building trust - with regulators, with customers, and with the people who use your product. Every swab, every air sample, every data point is a promise: We did everything we could to keep you safe. That’s not just quality control. That’s responsibility.What is the main purpose of environmental monitoring in manufacturing?
The main purpose is to detect and control contamination sources - like microbes, particles, chemicals, or waterborne hazards - before they affect products. It’s not about testing the final product; it’s about ensuring the environment where it’s made is safe. This prevents recalls, protects consumer health, and ensures regulatory compliance.
Which zones in environmental monitoring are most critical?
Zone 1 - direct product contact surfaces - is the most critical. These include slicers, mixers, and filling nozzles, and should be sampled daily. But Zone 3 and 4 surfaces - like floors, drains, and carts - are surprisingly important. A study found they were responsible for 62% of contamination events, proving that even low-risk areas need attention.
How often should environmental sampling be done?
Sampling frequency depends on the zone and industry. Zone 1 surfaces in food or pharma are typically sampled daily or after each shift. Zone 2 is sampled weekly, Zone 3 monthly, and Zone 4 quarterly. FDA requires weekly Listeria testing in Zone 1 for ready-to-eat food facilities. Frequency should always be risk-based, not arbitrary.
What’s the difference between ATP testing and microbiological testing?
ATP testing detects organic residue - like food, sweat, or grease - and gives results in seconds. It tells you if a surface is visibly clean. Microbiological testing identifies actual pathogens like Listeria or Salmonella, but takes 24-72 hours. ATP is great for quick checks and turnaround; microbiological tests are required for regulatory compliance and to confirm safety.
Why do pharmaceutical facilities have stricter environmental standards than food plants?
Pharmaceutical products are often administered directly into the body - injections, inhalers, implants - with no natural defense against contamination. Even tiny amounts of microbes can cause serious infections. Food products are consumed, but the body has defenses like stomach acid. That’s why pharma requires ISO Class 5 cleanrooms, continuous air monitoring, and strict humidity control - standards far beyond what most food facilities need.
What are the biggest challenges in implementing environmental monitoring?
The top three challenges are: inconsistent sampling techniques (68% of facilities), unclear zone classification (42%), and poor integration of data from ATP, microbiological, and allergen tests (37%). Many facilities also underestimate Zone 3 and 4 areas, failing to see how they contribute to contamination spread. Training and data systems are key to solving these.
Is environmental monitoring only for large manufacturers?
No. While 98% of pharmaceutical manufacturers have formal programs, only 76% of food processors do - and just 48% of small facilities under 50 employees meet full compliance. Size doesn’t exempt you. Regulators inspect all facilities. A small facility can still cause a widespread outbreak. The same zone system, training, and basic testing apply - just scaled down. Start simple, stay consistent.






Posts Comments
mohit passi November 26, 2025 AT 15:36
This is why I love tech with soul 🌱
It’s not just about compliance - it’s about holding space for safety. Every swab is a silent promise to someone you’ll never meet. We’re not cleaning surfaces. We’re cleaning the world one zone at a time.
Aaron Whong November 28, 2025 AT 13:23
The paradigm shift from endpoint validation to real-time environmental intelligence is non-negotiable in GxP ecosystems. The confluence of ATP bioluminescence kinetics with NGS-based metagenomic surveillance represents a quantum leap in process analytical technology (PAT). Failure to integrate these modalities constitutes a critical deviation from ICH Q10 principles.
Deborah Williams November 28, 2025 AT 13:41
Oh wow, so now we’re treating factory floors like sacred temples? 🙄
Let me guess - next they’ll make us pray before we wipe down a conveyor belt?
Kaushik Das November 29, 2025 AT 20:01
Man, I’ve seen this play out in 3 different plants - Zone 3 is the silent killer. We had this one guy who’d bring his dog to the breakroom, then walk straight to the packaging line. No shoes, no change, no thought. One day, we found Bacillus subtilis in a juice carton. Turned out it was from the dog’s fur. We started requiring boot changes even for breakroom access after that. Small things, big consequences.
Rachel Whip November 30, 2025 AT 03:47
ATP testing is a game-changer for small teams. We went from 48-hour turnaround to same-day decisions. Our downtime dropped 40%. No fancy AI needed - just consistency and training. If your team doesn’t know how to swab properly, no tech will save you.
Ali Miller December 2, 2025 AT 01:52
This is why America is falling behind. Europe’s got their GMP Annex 1, China’s rolling out AI-driven monitoring in every factory, and we’re still arguing whether Zone 2 needs weekly swabs? We’re not protecting consumers - we’re protecting paperwork.
JAY OKE December 2, 2025 AT 21:42
I work in a small food plant. We don’t have a budget for NGS or AI. But we do have a whiteboard, a checklist, and a guy who checks the drain every morning. It’s not glamorous. But we haven’t had a recall in 5 years. Sometimes simple beats sexy.
Joe bailey December 3, 2025 AT 17:07
This is the stuff that matters. Not the headlines. Not the stock prices. This right here - the swabs, the logs, the quiet people who check the floor before shift change - this is what keeps people alive. 🙌
Shoutout to the unsung heroes in PPE who never get a thank you.
Amanda Wong December 4, 2025 AT 11:30
All this ‘risk mapping’ is just corporate theater. If regulators really cared, they’d shut down every facility that uses plastic pallets. They know it’s a contamination vector. But they don’t. Because they’re paid by the same companies they inspect.
Stephen Adeyanju December 5, 2025 AT 11:41
Zone 4 is a scam they made up so we’d buy more swabs
Who cares if someone walks in from the parking lot
People touch doorknobs all day
Its not the floor its the people
james thomas December 6, 2025 AT 05:50
They say contamination control is a competitive advantage. Nah. It’s a tax. Big pharma pushes this so small shops can’t afford to compete. If you’re not spending $200k a year on monitoring, you’re not ‘serious’. But guess what - most outbreaks come from big players with fancy labs. The system’s broken.
Write a comment