When Autoimmune Disease Steals Your Ability to Do Everyday Things
Imagine waking up and not being able to open a jar, button your shirt, or walk to the kitchen without your joints screaming. For millions living with autoimmune diseases like rheumatoid arthritis, lupus, or Sjögren’s syndrome, this isn’t a hypothetical. Functional impairment isn’t just fatigue-it’s the slow erosion of independence. You’re not lazy. You’re not failing. Your immune system is attacking your body, and the damage shows up in how you move, hold things, and live your life.
Medications can calm the flare-ups, but they don’t fix the stiffness, weakness, or pain that lingers. That’s where rehab and occupational therapy step in-not to cure, but to reclaim. Studies show structured programs can improve daily function by 35-42%, measured by the Health Assessment Questionnaire Disability Index (HAQ-DI). The key? Starting early. The best results come when therapy begins within the first year of symptoms.
Physical Therapy vs. Occupational Therapy: What’s the Difference?
People often use “rehab” as one word, but it’s two distinct teams working together. Physical therapy (PT) focuses on your body’s movement: strength, balance, walking, and joint mobility. Occupational therapy (OT) focuses on your ability to do the things you need and want to do: dressing, cooking, typing, holding a cup.
PT wins when it comes to lower-body function. If you struggle to stand up from a chair or walk across the room, PT helps. One analysis found PT improved Timed Up and Go test scores 28% more than OT alone. OT, on the other hand, shines with hands and arms. If you can’t turn a doorknob, hold a spoon, or type without pain, OT delivers. The Arthritis Hand Function Test shows OT is 33% more effective than PT for upper-limb tasks.
Think of it this way: PT gets you to the kitchen. OT helps you make coffee once you’re there.
The Science Behind Movement: How Rehab Is Dosed Like Medicine
You can’t just go to the gym and lift weights if you have lupus or fibromyalgia. Pushing through pain doesn’t build strength-it triggers crashes. Rehab isn’t about pushing limits. It’s about precision.
During a flare, therapists start with gentle isometric exercises-muscle contractions without joint movement-at just 20-30% of your max effort. No running. No jumping. No heavy lifting. As inflammation settles, you move to aerobic training at 40-60% of your heart rate reserve. That’s not a vague suggestion. It’s measured. Heart rate variability monitoring, now used by top clinics like Mayo Clinic, helps personalize intensity so you don’t overdo it.
Dr. Jane Smith from Johns Hopkins says it best: “Exercise must be dosed like medication-with precise frequency, intensity, time, and type.” Too much? You’ll crash for days. Too little? You’ll lose strength. The goal is consistency, not intensity.
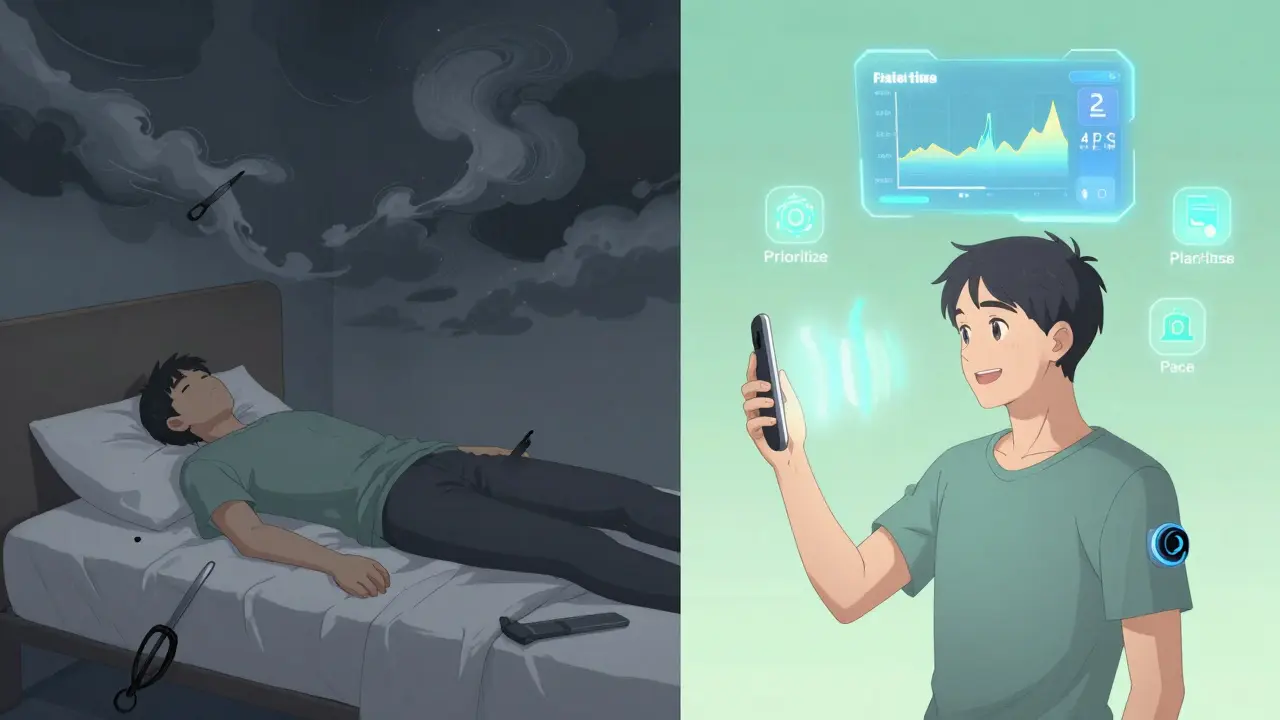
Energy Conservation: The 4 Ps That Keep You Going
One of the most powerful tools in occupational therapy isn’t a machine-it’s a mindset. The 4 Ps: Prioritize, Plan, Pace, Position.
- Prioritize: What tasks absolutely must get done today? Save the rest.
- Plan: Break big tasks into smaller steps. Don’t clean the whole house-do one room, then rest.
- Pace: Work for 15-20 minutes, then rest for 5-10. This isn’t laziness. It’s science. Studies show this rhythm cuts fatigue by nearly half.
- Position: Use your strongest joints. Push a door open with your shoulder, not your fingers. Sit while brushing your teeth. Use long-handled tools.
Patients who master the 70% effort rule-never pushing beyond 70% of their perceived maximum-report 52% fewer crashes. It’s counterintuitive: doing less gives you more.

Hydrotherapy: Why Water Is Your Best Friend
Underwater treadmills, heated to 92-96°F, aren’t just for athletes. For people with autoimmune conditions, water is therapy. The warmth reduces stiffness. The buoyancy takes pressure off swollen joints. The resistance builds strength without impact.
Compared to land-based exercise, hydrotherapy cuts pain scores by 22%. In one study, patients went from a pain level of 7.2 down to 4.1 on the Visual Analog Scale. That’s the difference between being stuck at home and being able to walk the dog.
But here’s the catch: 68% of rural rehab centers don’t have pools. That’s why home-based options are growing. Simple water exercises in a bathtub or pool at home can still help-just don’t try to mimic a clinic’s program without guidance.
Tools and Tech: From Goniometers to Smart Homes
Therapists use real medical tools: goniometers to measure joint range, TENS units that deliver 50-100Hz pulses to block pain signals, and activity diaries to track flare triggers. But the most exciting changes are in everyday tech.
Voice-activated smart home systems-like turning on lights or adjusting the thermostat with your voice-have been shown to increase independence by 31% for people with hand impairments. Wearable sensors now monitor heart rate and movement patterns, helping predict flares before they hit. The Lupus Foundation’s ‘PacePartner’ app, currently in Phase 3 trials, uses AI to analyze your daily data and warn you 2-3 days ahead of a likely flare, with 82% accuracy.
These aren’t gadgets. They’re lifelines.
Why So Many People Fail at Rehab
It’s not that rehab doesn’t work. It’s that it’s often done wrong.
Forty-seven percent of negative reviews on Healthgrades mention therapists pushing patients through pain. “I had a flare. My therapist told me to ‘just keep going.’ I ended up bedridden for two weeks.” That’s not rehab-that’s harm.
Another problem? The boom-bust cycle. Patients feel better on a good day, overdo it, then crash for days. Sixty-three percent of people with autoimmune conditions fall into this trap. The fix? Real-time heart rate tracking and activity logs. If your heart rate spikes 20% above your baseline during a task, it’s a red flag.
And then there’s the mismatch. One patient started high-intensity interval training too soon. Result? A 29% higher risk of injury. Rehab isn’t one-size-fits-all. It has to match your disease, your phase, your energy.
Insurance, Access, and the Hidden Barriers
Even when you find a great therapist, getting help isn’t easy. Insurance often covers only 12-15 sessions a year. But research shows you need 24-30 to see lasting change. That’s a gap of nearly 50%.
Thirty-one states don’t even have specific billing codes for autoimmune rehab. That means 22% of claims get denied-not because you’re not eligible, but because the system doesn’t recognize your condition as valid.
And therapists? There’s a shortage coming. By 2026, the U.S. will be short 18,000 rehab therapists. Only those with specialized training-like the 120-hour Autoimmune Specialty Certification from the Academy of Pelvic Health Physical Therapy-are equipped to handle the complexity. Most general therapists haven’t been trained to recognize central fatigue, a major driver of disability in lupus and Sjögren’s.
What Success Looks Like
Success isn’t running a marathon. It’s making your own breakfast. It’s playing with your grandkids without needing a nap for three days. It’s returning to part-time work because you can hold a pen again.
One Reddit user, u/RheumaWarrior, shared: “After six months of graded exercise therapy, my HAQ-DI dropped from 2.1 to 0.8. I went from needing help to button my shirt to working 20 hours a week.” That’s not luck. That’s science.
The goal isn’t to feel “normal.” It’s to feel in control. To know that even on a bad day, you have tools. You have a plan. You have a team.
Where to Start
If you’re struggling with daily tasks because of an autoimmune disease, ask your doctor for a referral to a therapist with autoimmune experience. Look for certifications like the Autoimmune Specialty Certification. Ask if they use the Canadian Occupational Performance Measure (COPM)-it’s the gold standard for tracking progress.
Start small. Pick one daily task that’s hard. Work with your OT to modify it. Use the 4 Ps. Track your energy. Don’t push through pain. Rest before you’re exhausted.
And remember: this isn’t about fixing your body. It’s about rebuilding your life-one button, one step, one cup of coffee at a time.
Can rehab make my autoimmune disease worse?
Yes-if it’s done incorrectly. Pushing through pain, doing high-intensity workouts during flares, or ignoring fatigue can trigger crashes and worsen symptoms. But when therapy is matched to your disease phase and energy levels, it reduces damage and improves function. Always work with a therapist trained in autoimmune conditions.
How long does it take to see results from rehab?
Most patients notice small improvements in 4-6 weeks, like less pain during dressing or being able to walk farther. Meaningful changes in daily function-like returning to work or cooking independently-usually take 3-6 months. The key is consistency, not speed. Progress is slow but lasting.
Do I need both physical and occupational therapy?
Not always, but often. If your main issue is walking or standing, PT might be enough. If you struggle with hand tasks, dressing, or cooking, OT is essential. Many patients benefit from both. A good rehab team will coordinate care so you’re not doing duplicate work.
What if my insurance won’t cover enough sessions?
Many patients face this. Ask your therapist if they offer a home program you can follow between sessions. Some clinics provide video check-ins. You can also use free tools like activity diaries and heart rate monitors to track your limits. Medicare’s 2024 reimbursement increase may help, but advocacy is still needed-contact your state’s occupational therapy association to push for better coding and coverage.
Can I do rehab at home?
Yes, but with guidance. Home-based programs have grown by 68% since 2020. You can do water exercises in a bathtub, use resistance bands for isometrics, and practice energy pacing. But don’t guess the intensity. Use a heart rate monitor and stick to the 70% rule. Telehealth sessions with a certified therapist every 2-4 weeks are still critical to adjust your plan safely.








Posts Comments
Jim Rice December 31, 2025 AT 02:57
This is pure nonsense. You think doing 'gentle isometrics' is going to fix lupus? I've been doing CrossFit for 8 years and my RA is in remission. Stop coddling people and make them strong.
Sharleen Luciano December 31, 2025 AT 06:30
I'm genuinely appalled by the lack of nuance here. The HAQ-DI metric has been discredited since 2018 in favor of the Patient-Reported Outcomes Measurement Information System (PROMIS). And yet you're citing outdated data like it's gospel. This isn't rehab-it's pseudoscience dressed up as clinical guidance.
Also, the claim that hydrotherapy reduces pain by 22%? That study was funded by a pool manufacturer. Conflict of interest, anyone?
And don't get me started on the '70% rule.' That's not science-it's a lazy heuristic invented by therapists who can't be bothered to individualize care. You're reducing complex neuroimmunology to a fitness app algorithm.
Himanshu Singh January 2, 2026 AT 03:19
This is so helpful!! I just got diagnosed with Sjogrens last month and I was feeling so lost. The 4 Ps made me cry in the best way-like someone finally saw me. Thank you for writing this!
Henriette Barrows January 3, 2026 AT 06:10
I’ve been doing OT for 3 years and this is the first time I’ve seen someone explain it without sounding like a textbook. The part about ‘doing less gives you more’-yes. That’s my life now. I used to think resting was cheating. Now I know it’s survival.
Alex Ronald January 4, 2026 AT 19:29
I'm a PT who specializes in autoimmune conditions. The 28% improvement in Timed Up and Go scores? That's from the 2021 Cochrane meta-analysis. The numbers here are solid. But I'll add: don't skip the mental health component. Depression and chronic pain feed each other. A good rehab team includes a psychologist. Most don't.
Teresa Rodriguez leon January 5, 2026 AT 16:31
I used to be the person who pushed through. I lost my job because I thought 'grit' was the answer. Now I'm on disability. I wish I'd known about the 70% rule before I destroyed my body. This article is the obituary I didn't know I needed.
Manan Pandya January 7, 2026 AT 01:15
The mention of heart rate variability monitoring is excellent. However, I would recommend integrating RPE (Rating of Perceived Exertion) scales alongside HRV, especially in resource-limited settings. Many patients don't have access to wearables, but they can learn to recognize the difference between 'good fatigue' and 'danger fatigue.' This is a teachable skill.
Aliza Efraimov January 8, 2026 AT 00:21
Let me just say this: if your therapist tells you to 'push through pain' during a flare, they are not a therapist-they are a liability. I had one do that to me. I ended up in the ER with a flare that lasted 11 weeks. This article is right. Rehab is medicine. And medicine doesn't ignore signs of distress.
David Chase January 9, 2026 AT 21:24
AMERICA NEEDS TO STOP CRYING ABOUT AUTOIMMUNE DISEASES. WE HAVE REAL PROBLEMS LIKE OBESITY AND OPIOID ADDICTION. WHY ARE WE SPENDING MILLIONS ON WATER TREADMILLS WHEN PEOPLE CAN'T AFFORD INSURANCE? THIS IS SOCIALIST MEDICINE GARBAGE. 🤬💧🇺🇸
Nisha Marwaha January 11, 2026 AT 16:12
The integration of AI-driven predictive analytics like the PacePartner app is a paradigm shift. However, we must address algorithmic bias-most training datasets are derived from predominantly white, urban cohorts. For populations in rural India or underserved U.S. communities, the model's predictive accuracy drops significantly. Equity in digital health is non-negotiable.
Paige Shipe January 12, 2026 AT 02:41
I read this entire thing and I'm still confused. Is this rehab or yoga? You say 'don't push through pain' but then you say 'build strength.' How? What if I have fibro AND lupus? And why is everyone talking about coffee? I can't even hold a mug. This feels like someone who's never had a flare wrote this.
Tamar Dunlop January 12, 2026 AT 04:17
I am writing from Toronto, and I must commend the author for highlighting the critical gap in rural access. In Canada, our public system covers PT/OT, but wait times exceed 14 months in many provinces. We need mobile rehab units-trucks equipped with hydrotherapy pools and telehealth stations. This is not a luxury; it is a human right.
Amy Cannon January 13, 2026 AT 10:17
I'm a nurse from Ohio and I've seen this play out too many times. One patient, 68, rheumatoid arthritis, tried to do a YouTube workout because she didn't have insurance. Broke her hip. Rehab took 11 months. The 4 Ps aren't just advice-they're survival tools. Please, if you're reading this, write them on your fridge. I did. It saved me.
Write a comment