Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t accidents-they’re preventable. The real issue isn’t always the drugs themselves, but how they’re being used alongside habits that make them less safe-or even unnecessary.
You’re not alone if you’re taking multiple pills every day. For people over 65, it’s common to be on five or more medications. That’s called polypharmacy, and it triples your risk of dangerous side effects, falls, confusion, and hospital stays. But here’s the truth most doctors won’t tell you: some of those pills might not be needed at all-if you change the way you live.
Food Can Be Your First Medicine
What you eat doesn’t just affect your weight. It directly changes how your body responds to medication. For high blood pressure, cutting sodium from 3,500 mg to 1,500 mg a day can lower your numbers as much as a single pill. That’s not a guess-it’s from the New England Journal of Medicine. The DASH diet (Dietary Approaches to Stop Hypertension) was designed by researchers specifically to mimic the effect of antihypertensive drugs, without the side effects.
For Type 2 diabetes, a well-planned diet can bring blood sugar down as effectively as metformin. Losing just 5-7% of your body weight through food changes can cut diabetes medication needs by up to 60% in people with prediabetes. That’s not magic. It’s biology. When fat around your liver and pancreas goes down, your body starts using insulin properly again.
But not all healthy foods play nice with meds. Grapefruit can make statins too strong-sometimes dangerously so. Leafy greens like spinach and kale are full of vitamin K, which can mess with blood thinners like warfarin. Dairy can block antibiotics like tetracycline from being absorbed. That’s why talking to your pharmacist isn’t optional. They know what foods fight with your pills. Ask them: “Which of my foods could be hurting my meds?”
Movement Isn’t Optional-It’s Medication
Brisk walking for 30 minutes, three times a week, isn’t just good for your mood. It’s a proven way to lower blood pressure. When your heart gets stronger, it doesn’t have to work as hard. That means your body needs less medication to keep pressure under control.
One man from Bristol, who goes by “HypertensionWarrior” on Reddit, dropped his blood pressure from 150/95 to 125/80 in six months. He didn’t add a new pill. He started walking every morning and cut salt from his meals. His doctor took him off one medication. That’s not rare. It’s repeatable.
The American Heart Association recommends 150 minutes of moderate exercise a week-that’s 30 minutes, five days. Add two days of light strength training (lifting groceries, doing bodyweight squats, using resistance bands) and you’re doing more than most people on pills. Exercise doesn’t just lower blood pressure. It improves insulin sensitivity, reduces inflammation, and helps your liver process drugs more cleanly.
And you don’t need a gym. Park farther away. Take the stairs. Dance while you cook. Movement adds up. The key is consistency, not intensity.
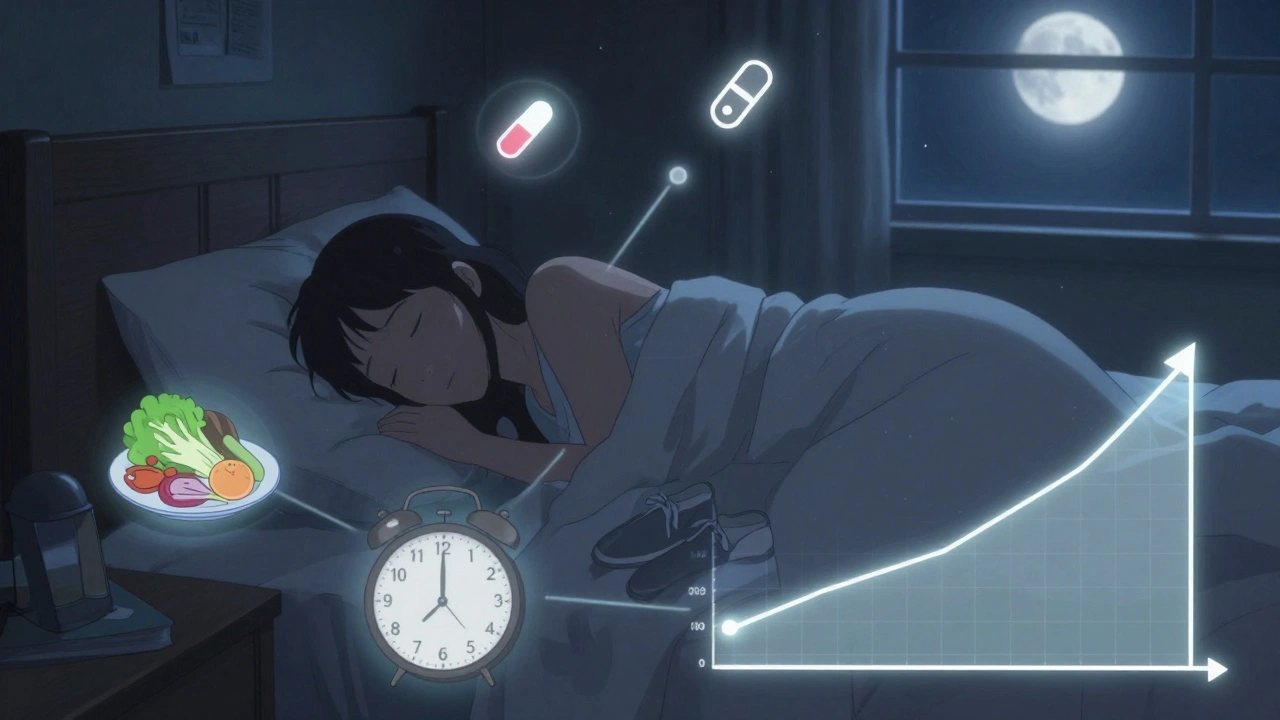
Sleep Is a Silent Drug Regulator
If you’re sleeping less than seven hours a night, you’re making your medications less effective-and your body more vulnerable. Chronic sleep loss raises cortisol, which spikes blood sugar and blood pressure. It also increases inflammation, which is linked to heart disease, arthritis, and even depression.
Studies show people who sleep poorly are 40% more likely to need higher doses of diabetes meds. They’re also more likely to experience side effects from blood pressure pills, like dizziness or fatigue. Why? Because your body can’t repair itself properly without deep sleep.
Fixing sleep doesn’t mean buying a $2,000 mattress. It means: no screens 90 minutes before bed, keeping your room cool (around 18°C), and going to bed and waking up at the same time-even on weekends. Try it for two weeks. You might find you need less of that nighttime anxiety pill.

Stress, Smoking, and Alcohol-The Hidden Med Risks
Chronic stress keeps your body in fight-or-flight mode. That means your heart races, your blood pressure climbs, and your blood sugar spikes. All of that makes your meds work harder. And if you’re taking beta-blockers or antidepressants, stress can make them less effective.
Yoga, meditation, or even five minutes of deep breathing a day can lower blood pressure and reduce anxiety without adding another pill. The Michigan State University College of Pharmacy says stress management is just as important as diet and exercise for heart health.
Smoking? It makes your blood thicker, your arteries stiffer, and your liver work overtime to clear drugs. If you’re on blood thinners, statins, or insulin, smoking cuts their effectiveness. Quitting doesn’t just reduce your risk of heart attack-it can cut your medication needs in half over time.
Alcohol is trickier. One drink a day for women, two for men, might be okay. But if you’re on painkillers, antidepressants, or sleep aids, even one drink can be dangerous. Alcohol and acetaminophen together can damage your liver. Alcohol and benzodiazepines can slow your breathing to a stop. If you’re unsure, ask your pharmacist: “Is my drink safe with my pills?”
Don’t Stop Your Meds-Work With Your Doctor
Lifestyle changes don’t replace medication. They make it safer and sometimes less needed. Never quit a pill because you feel better. That’s how people end up in the hospital.
Dr. Rob Shmerling from Harvard Health says: “Medications should be in addition to lifestyle changes, not instead of them.” That’s the rule.
But here’s how to make progress: keep a journal. Write down your daily walks, what you ate, how much you slept, and how you felt. Bring it to your doctor every three months. Ask: “Are there any meds I could reduce?”
One woman in her 60s reduced her diabetes pills from three to one after six months of walking, eating more veggies, and sleeping better. Her doctor didn’t push it-he just watched the numbers. Her HbA1c dropped from 7.8% to 6.1%. That’s not a miracle. That’s science.
What’s Holding You Back?
People say they don’t have time. But 30 minutes of walking is less than a Netflix episode. They say healthy food is expensive. But beans, oats, eggs, and frozen veggies cost less than processed snacks and sugary drinks. They say they’ll start tomorrow. But tomorrow never comes.
Start small. Pick one thing. Walk every day for 10 minutes. Swap soda for water. Go to bed 30 minutes earlier. Do that for two weeks. Then add another.
The American College of Lifestyle Medicine has over 12,000 certified practitioners now. They’re not trying to replace doctors. They’re helping people take back control. And it’s working. Employers who offer lifestyle programs see 18.7% lower healthcare costs. Medicare Advantage plans now cover these programs. The FDA is starting to require lifestyle data when approving new drugs for diabetes and heart disease.
You don’t need to be perfect. You just need to be consistent. Every step you take toward better sleep, better food, and more movement doesn’t just reduce your risk of side effects-it gives you your life back.
What to Do Next
- Write down every medication you take, including vitamins and supplements.
- Ask your pharmacist: “Which foods or drinks should I avoid with these?”
- Start one new habit: walk 10 minutes a day, or swap one sugary snack for fruit.
- Track your progress for 30 days-no judgment, just observation.
- Bring your notes to your doctor and ask: “Could any of these meds be reduced if I stick with these changes?”
Medications save lives. But they’re not the only tool. The best outcomes come when pills and habits work together. You don’t need to be a health expert. You just need to start.
Can lifestyle changes really replace my medications?
No, lifestyle changes shouldn’t replace medications unless your doctor says so. But they can reduce how much you need. For example, losing weight and eating well can cut diabetes pill doses by 40-60% in some cases. Always work with your doctor before making any changes.
How long does it take to see results from lifestyle changes?
It usually takes 3-6 months to see measurable changes in blood pressure, blood sugar, or cholesterol. Some people notice feeling better in weeks-more energy, better sleep-but lab numbers take time. Don’t give up before the 90-day mark.
Is it safe to cut back on meds if I feel better?
Never stop or reduce a medication on your own. Even if you feel fine, stopping suddenly can cause dangerous rebounds-like a spike in blood pressure or blood sugar. Always talk to your doctor first. Use your lifestyle journal to show progress, then ask if a reduction is possible.
What if I can’t afford healthy food or gym membership?
You don’t need expensive food or a gym. Frozen vegetables, beans, eggs, oats, and seasonal fruit are affordable. Walking, bodyweight exercises, and stretching at home cost nothing. Focus on what you can do, not what you can’t. Small steps still move the needle.
Do I need to change everything at once?
No. Trying to overhaul your life in a week leads to burnout. Pick one thing-like drinking more water or walking after dinner-and stick with it for two weeks. Then add another. Progress is slower than you think, but it’s lasting.
Can I still drink alcohol or coffee with my meds?
It depends. Coffee is usually fine unless you’re on certain antidepressants or heart meds. Alcohol can be dangerous with painkillers, sleep aids, or blood thinners. Ask your pharmacist about each medication you take. They’ll tell you what’s safe and what’s risky.
Why don’t doctors talk more about lifestyle changes?
Many doctors want to, but time is short. Visits are 10-15 minutes. Also, not all doctors are trained in lifestyle medicine-it’s still growing in medical schools. But that’s changing. More clinics now have nutritionists and health coaches. Ask if your doctor can refer you to one.
What if I slip up? Does it ruin everything?
No. Health isn’t about perfection. It’s about patterns. One bad meal or missed walk doesn’t undo progress. What matters is getting back on track. Most people who succeed don’t do it perfectly-they just keep going.








Posts Comments
Ashley Farmer December 7, 2025 AT 11:55
It’s so refreshing to see someone lay this out without sugarcoating. I’ve been helping my mom manage her meds for years, and the food interactions were never mentioned until we talked to her pharmacist. Grapefruit and her statin? Total surprise. Now she avoids it completely and her liver numbers improved. Small changes, huge impact.
Helen Maples December 7, 2025 AT 19:15
This article is accurate but incomplete. The systemic failure here isn’t patient ignorance-it’s medical training. Doctors are incentivized to prescribe, not to educate. Medical schools spend 20 hours on nutrition in four years. Twenty. Meanwhile, pharmaceutical reps visit them daily. No wonder people end up on ten pills when three would do with lifestyle intervention. The system is broken, and patients are paying the price.
David Brooks December 9, 2025 AT 05:15
OMG I just did what this article said and I’m crying right now. I cut out soda, started walking after dinner, and slept seven hours for a week. My blood pressure dropped 18 points. My doctor looked at me like I’d grown a second head. I didn’t take a single new pill. I just moved and ate better. I feel like a new person. This isn’t hype-it’s HOPE.
Jennifer Anderson December 10, 2025 AT 15:52
sooo i started doing the 10 min walk thing and honestly? i didnt think itd do anything. but after two weeks i slept better and my knee pain got way less. i didnt even realize how much i was dragging myself around. now i do 15. no gym. no fancy gear. just me and my sneakers. also swapped my afternoon candy bar for an apple. no regrets. 🍎
Sadie Nastor December 12, 2025 AT 00:14
Thank you for writing this. I’ve been scared to even ask my doctor about cutting meds because I thought I’d be judged. But your note about keeping a journal? That’s genius. I started tracking my walks, meals, and sleep last month. Just notes. No pressure. I showed it to my doctor last week and she said, ‘Let’s try reducing the sleep aid.’ I cried. Not from sadness-from relief. You don’t have to fix everything at once. Just show up.
Nicholas Heer December 12, 2025 AT 01:29
THIS IS A BIG PHARMA LIE. They don’t want you to heal naturally because pills = profits. They fund the ‘studies’ that say lifestyle doesn’t work. The FDA? Bought and paid for. The WHO? Controlled by the same shadow corps that own the drug companies. They’ll never admit that walking and broccoli can outperform their $200-a-pill miracle drugs. Wake up. The real epidemic isn’t hypertension-it’s corporate control of your health.
Sangram Lavte December 12, 2025 AT 17:00
I live in India, and this is so relevant here too. Many people think medicine is the only solution, but we’ve had Ayurveda and traditional diets for centuries. Eating whole grains, walking daily, sleeping early-these aren’t new. They’re forgotten. I’ve seen relatives reduce their diabetes meds after switching to millet and lentils instead of white rice. No magic. Just return to basics. The science is just catching up.
Oliver Damon December 14, 2025 AT 14:51
What’s fascinating here is the epistemic shift: we’re moving from a pharmacological paradigm to a physiological one. The body isn’t a machine that needs replacement parts-it’s an ecosystem that needs balance. Medications are bandages. Lifestyle is healing. The real challenge isn’t adherence-it’s re-educating a medical culture that conflates intervention with care. We treat symptoms because we’ve lost the language of root causes. This article doesn’t just offer advice-it offers a new framework for health.
Write a comment