When a patient walks out of the clinic with a new prescription, they’re not just getting a pill-they’re getting a promise. A promise that it will work. That it won’t break the bank. That they can take it every day without fear or confusion. But too often, that promise falls apart before they even get to the pharmacy. Why? Because generic medications are still misunderstood-even by the people who need them most.
Healthcare providers are in a unique position to change that. Not by pushing pills, but by having real conversations. By explaining, not assuming. By listening, not lecturing. Because when patients trust their doctor or pharmacist, they’re far more likely to stick with a generic drug-even if it looks different, costs less, or comes in a different shape.
Why Generics Matter More Than Ever
Over 90% of prescriptions filled in the U.S. are for generic drugs. Yet they make up just 23% of total drug spending. That’s not a fluke. It’s proof that generics save money-big time. Within a year of a brand-name drug losing patent protection, its generic version typically costs just 15% of the original price. For patients on fixed incomes, chronic conditions like diabetes or high blood pressure, that difference isn’t just helpful-it’s life-changing.
But here’s the catch: patients who can’t afford their meds don’t just skip doses. They stop entirely. A 2019 analysis of over 1.4 billion prescriptions found that patients were 266% more likely to abandon a brand-name drug than a generic one. Why? Because 90% of generic copays were under $20. Meanwhile, 39% of brand-name copays were over $20. That’s not a small gap. It’s a cliff.
And it’s not just about price. When patients stop taking their meds because they can’t afford them, their health crashes. Hospital visits spike. Costs go up-for them, for the system, for everyone. Providers who ignore this aren’t just missing a chance to save money. They’re missing a chance to save lives.
The Science Behind Generics Is Rock Solid
Patients hear rumors. “Generics aren’t as strong.” “They don’t work the same.” “I switched and felt weird.” These aren’t just myths-they’re barriers. And they’re hard to break.
The truth? The FDA requires generics to meet the same strict standards as brand-name drugs. They must have the same active ingredient, strength, dosage form, and route of administration. And they must prove bioequivalence: meaning the body absorbs them at the same rate and to the same extent as the brand. The acceptable range? Between 80% and 125% of the brand’s absorption. That’s not a guess. That’s science.
Yes, generics can look different. Different color. Different shape. Different filler ingredients. But those changes don’t affect how the drug works. They’re just there to avoid patent issues. And the FDA checks every batch. Every lot. Every manufacturer. If a generic fails, it doesn’t hit the market.
Still, patients don’t trust the system. They trust their provider. That’s the key.
Provider Advocacy Isn’t Optional-It’s Essential
The American College of Physicians and the American Academy of Family Physicians both agree: doctors should prescribe generics whenever possible. But they also know it’s not that simple. Some drugs-like blood thinners or seizure meds-have a narrow therapeutic index. That means tiny changes in absorption can cause big problems. For those, providers need to be extra careful. But for the vast majority of medications? Generics are safe, effective, and cheaper.
So why don’t all providers push them? Time. Stress. Assumptions. Many think, “They’ll figure it out at the pharmacy.” But patients don’t. They see a new pill. It’s blue instead of green. It says “Watson” instead of “Pfizer.” They panic. They call their doctor. They stop taking it. They think something’s wrong.
That’s where advocacy comes in. Not just prescribing generics-but talking about them. Proactively. Clearly. Without jargon.
Here’s what works:
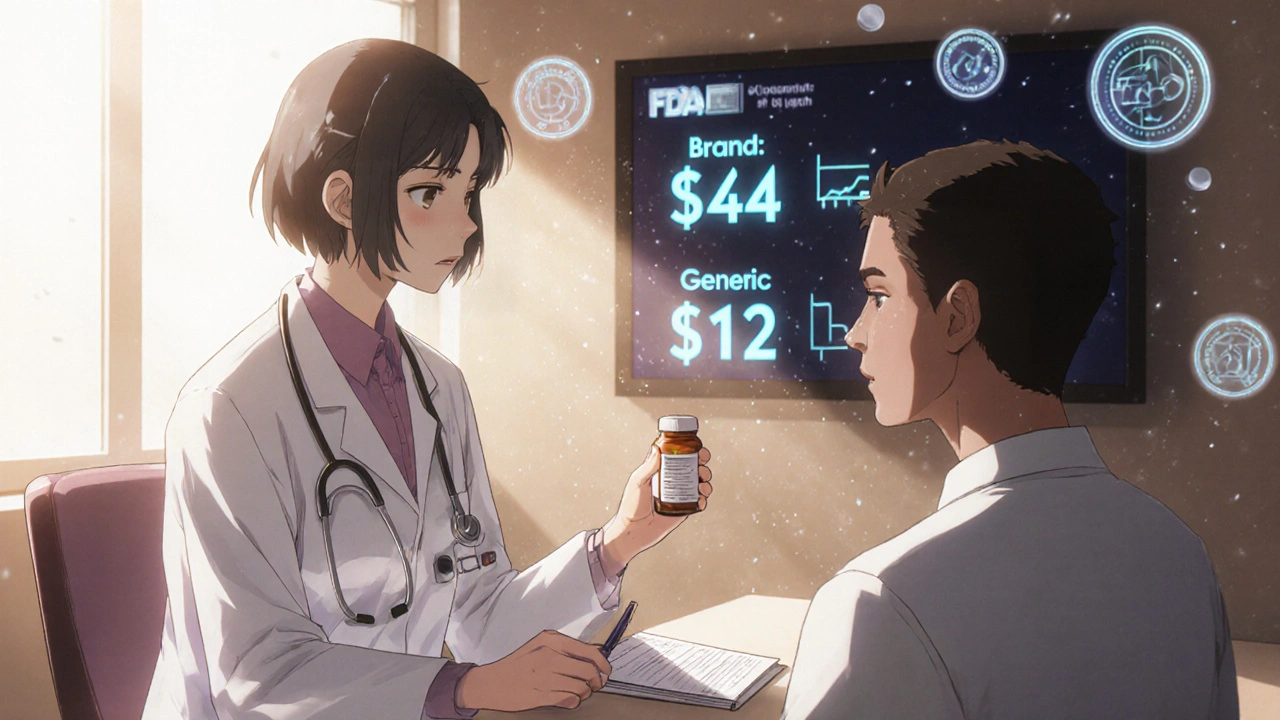
- “This is a generic version of your old pill. It has the same active ingredient, but it’s cheaper-your copay drops from $45 to $12.” (Say the numbers. Patients hear numbers.)
- “It might look different, but it’s just as safe and effective. The FDA checks it just like the brand-name one.” (Name the authority. It builds trust.)
- “I’ve prescribed this to dozens of patients. No one had problems. But if you feel anything unusual, call me right away.” (Offer reassurance, not dismissal.)
Pharmacists play a huge role too. In fact, the FDA says pharmacists have “such a large impact on patients when it comes to generic drug literacy.” But if the provider doesn’t set the tone, the pharmacist is playing catch-up. A simple note on the prescription-“Patient counseled on generic substitution”-makes a difference.
When Generics Don’t Work-And What to Do About It
There are rare cases where a patient genuinely doesn’t tolerate a generic. Maybe they’ve been on the same brand for 10 years. Maybe they’re sensitive to a filler. Maybe they’ve had bad experiences before. That’s real. And it’s valid.
But here’s the mistake: assuming it’s the generic’s fault without checking. Sometimes, the issue isn’t the drug-it’s the switch. Patients get switched back and forth between different generic manufacturers over the year. One looks like a blue oval. Another is a white circle. They get confused. They think the new one isn’t working. But it’s the same drug. Just a different look.
Best practice? When switching, explain it. Say: “Your prescription might come from different companies over time. They all have the same medicine inside. The color or shape might change, but the effect won’t.”
And if a patient truly can’t tolerate a generic? Document it. Write “brand necessary due to patient intolerance” on the prescription. Don’t just say “no generics.” Be specific. That protects the patient and helps future providers.
The American Academy of Family Physicians opposes mandatory generic substitution for this exact reason. Advocacy isn’t about forcing choices. It’s about empowering them.
The Hidden Cost of Silence
Every time a provider doesn’t explain a generic, they’re not just saving 30 seconds. They’re risking a cascade of consequences.
- Patient stops taking meds → blood pressure spikes → ER visit → $12,000 bill
- Patient misses insulin doses → diabetic complication → amputation risk
- Patient stops antidepressant → depression worsens → lost work, strained relationships
These aren’t hypotheticals. They happen every day. And they’re preventable.
Providers aren’t just prescribers. They’re advocates. And advocacy means speaking up-not just for the drug, but for the person.
One study found that when patients trusted their doctor’s opinion on generics, they were far more likely to accept them-even if they’d previously refused. That’s the multiplier effect. One conversation. One moment of clarity. It ripples.
What’s Changing Now-and What’s Next
The landscape is shifting. Some generic drugs, especially older ones, are seeing price spikes. The American Society of Health-System Pharmacists warned in 2023 that rising costs for certain generics could lead to “serious public health consequences.” That’s new. That’s alarming. And it means providers need to be even more vigilant.
Not all generics are cheap anymore. But most still are. And for the ones that aren’t? Providers need to know why. Is it a shortage? A patent issue? A manufacturing problem? That knowledge lets them make better choices-for the patient, not just the system.
Electronic health records are starting to show real-time cost data at the point of prescribing. Soon, a doctor might see: “Generic available. Copay: $8. Brand: $52.” That’s powerful. But only if the provider uses it. Only if they say: “This will cost you less than your coffee each day.”
The future of patient advocacy isn’t about lobbying or policy. It’s about daily conversations. It’s about looking a patient in the eye and saying: “I know this isn’t the brand you’re used to. But I’ve seen people like you do great on this. Let me explain why.”
That’s not just good medicine. It’s the kind of care people remember.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning the body absorbs them at the same rate and to the same extent. Studies show no difference in clinical outcomes for the vast majority of medications. The FDA holds generics to the same quality standards as brand-name drugs.
Why do generic pills look different from brand-name ones?
Generic drugs must differ in appearance to avoid infringing on the brand’s trademark. That means different colors, shapes, or markings. But those changes only affect how the pill looks or tastes-not how it works. The active ingredient is identical. The FDA allows these differences as long as they don’t impact safety or effectiveness.
Can switching to a generic cause side effects?
Rarely. Most side effects are due to the active ingredient, which doesn’t change between brand and generic. But some patients may react to inactive ingredients-like fillers or dyes-used in a specific generic version. If a patient notices new symptoms after switching, it’s worth checking. But it’s not the norm. Providers should ask about changes in how the patient feels after any switch.
Why do some doctors refuse to prescribe generics?
Some doctors avoid generics out of habit, lack of awareness, or concern about rare cases where interchangeability isn’t ideal-like with certain seizure or thyroid medications. Others may be influenced by pharmaceutical marketing. But professional guidelines from the American College of Physicians and others now strongly recommend prescribing generics unless there’s a clear clinical reason not to. Patient cost and adherence are major factors.
How can I talk to my patient about switching to a generic without sounding dismissive?
Start by acknowledging their experience: “I know you’ve been on this brand for a while, and it’s worked for you.” Then explain: “The generic has the same medicine inside, but it’s much cheaper-your copay drops from $45 to $12. Many patients switch without any issues. The FDA checks it just like the brand. If you notice anything unusual, let me know right away.” Frame it as a win-saving money without losing effectiveness.
Is it safe to switch between different generic manufacturers?
Yes. All FDA-approved generics must meet the same bioequivalence standards, no matter who makes them. But patients can get confused if their pill changes color or shape every refill. That’s why it’s important to explain upfront: “You might get different-looking pills over time, but they all contain the same medicine. If you’re unsure, check the name on the bottle-it will say the generic name, like ‘amlodipine,’ not the brand.”
Do generics take longer to work than brand-name drugs?
No. Bioequivalence testing ensures generics enter the bloodstream at the same rate and to the same extent as the brand. Studies show no meaningful difference in how quickly they start working. If a patient feels a delay, it’s more likely due to expectations or unrelated factors-not the drug itself.
Providers who take the time to explain generics don’t just reduce costs-they reduce fear. They reduce abandonment. They reduce hospitalizations. That’s the real impact. Not in a report. Not in a statistic. In a patient’s daily life.






Posts Comments
Laurie Sala November 24, 2025 AT 03:39
Ugh, I can't believe how many patients just quit their meds because the pill looks different!!! I had one lady cry because her blood pressure med went from pink to white-like it was a betrayal?? She thought the pharmacy gave her the wrong stuff. I had to sit with her for 20 minutes just to explain FDA bioequivalence. People are terrified of change, even when it's cheaper and safer. Why do we make them suffer because we won't talk?
Lisa Detanna November 24, 2025 AT 14:13
As someone who grew up in a household where medicine was a luxury, I can tell you-generics saved my mom’s life. She had diabetes, and that $50 copay for brand-name insulin? Impossible. The generic? $12. She lived 12 more years because someone finally explained it to her like a human, not a chart. Providers who don’t talk about this aren’t just lazy-they’re complicit in preventable suffering.
Demi-Louise Brown November 26, 2025 AT 04:28
The clinical evidence supporting generic medications is unequivocal. The FDA's bioequivalence standards are rigorously enforced, and multiple meta-analyses confirm no significant difference in therapeutic outcomes across the vast majority of drug classes. The primary barrier to adoption is not pharmacological, but psychological. Effective provider communication remains the most underutilized tool in improving adherence.
Matthew Mahar November 27, 2025 AT 08:30
Okay so I switched my dad to a generic for his cholesterol med and he got this weird blue pill instead of the green one he'd been on for 7 years and he THOUGHT he was being poisoned?? I had to drive to his house with the FDA website open on my laptop and read him the whole thing like a bedtime story. He cried. I cried. We both cried. And then he took it. And his numbers are better. But why does it have to be this hard??
John Mackaill November 28, 2025 AT 03:49
It’s not just about cost-it’s about dignity. When a patient can afford their meds, they feel seen. When they can’t, they feel discarded. I’ve had patients tell me they’d rather skip meals than skip pills. Generics aren’t a compromise. They’re justice. And if we’re not talking about them, we’re failing our moral duty.
Adrian Rios November 29, 2025 AT 16:04
Let’s be real here-most of us were never taught how to talk about generics in med school. We learned the science, sure, but not the art of the conversation. We got handed a script: ‘This is a generic.’ End of discussion. But patients aren’t robots. They need context. They need reassurance. They need to know you’re not just trying to cut costs-you’re trying to keep them alive. I started saying, ‘I’ve prescribed this to over 200 people. Not one had an issue. But if you feel off, I want you to call me. Not your pharmacist. Not Google. Me.’ And guess what? Compliance went up 40%. It’s not magic. It’s just being human.
Casper van Hoof November 29, 2025 AT 18:56
The epistemological framework underlying generic drug acceptance is predicated upon a paradox: while the pharmacological equivalence is empirically validated, the phenomenological experience of the patient remains culturally and psychologically distinct. The dissonance between scientific fact and subjective perception constitutes a hermeneutic gap that medical authority alone cannot bridge without hermeneutic humility.
Richard Wöhrl November 30, 2025 AT 12:27
Just wanted to add-this is why I always write ‘Patient counseled on generic substitution’ on the script, even if I’m not the one doing it. Pharmacists are heroes here. I had a patient come back last week because she was confused-her pill changed shape twice in one month. She thought it was a different drug. I didn’t know until she told me. So now, I tell patients upfront: ‘You might get different-looking pills. That’s normal. The name on the bottle is what matters-like ‘metformin,’ not ‘Glucophage.’ If you’re ever unsure, call me. Don’t guess.’ Simple. Clear. Saves lives.
Pramod Kumar December 1, 2025 AT 07:48
In India, we call generics ‘jugaad medicine’-clever, resourceful, life-saving. My grandmother took a generic for hypertension for 15 years. She never missed a dose. She never went to hospital. She danced at my wedding. The color? Yellow. The brand? Forgotten. The result? Alive. We don’t worship brands here-we worship results. Maybe the West needs to learn that too.
Henrik Stacke December 2, 2025 AT 05:10
There is a certain irony in the fact that, while the pharmaceutical industry is often vilified for its pricing practices, the very same industry has, through its patent protections, inadvertently created a system wherein the most effective tool for patient adherence-generic substitution-is rendered a matter of profound cultural anxiety. One might argue that the true pharmaceutical innovation lies not in molecular structure, but in communication.
Manjistha Roy December 2, 2025 AT 09:34
I work in a community clinic. We have a patient who refused generics for five years. Said she ‘felt weird’ on them. We finally sat down. Turned out she’d been switched between six different generic manufacturers. Each pill looked different. She thought the medicine was changing. We printed out a chart: same drug, different look. She cried. Now she takes it without question. It’s not about the pill. It’s about the fear. And fear needs a voice.
Jennifer Skolney December 2, 2025 AT 17:00
My mom’s on a generic for her antidepressant. She used to say, ‘It’s not the same.’ Now she says, ‘It’s the same, but I can afford to take it.’ That’s the whole story right there. 💙
JD Mette December 3, 2025 AT 22:36
I’ve seen patients stop meds because the generic had a different filler. One guy thought the cornstarch in his generic metformin was ‘giving him anxiety.’ He didn’t know cornstarch was in 80% of pills. We ran a test. Nothing. He just needed someone to say, ‘It’s okay to feel weird, but it’s probably not the drug.’ That’s all it took.
Write a comment