Most People Who Think They’re Allergic to Penicillin Aren’t
Almost 1 in 10 people in the U.S. say they’re allergic to penicillin. But here’s the truth: 9 out of 10 of those people aren’t actually allergic. This isn’t a small mistake-it’s a public health issue with real consequences. When doctors avoid penicillin because a patient says they’re allergic, they often turn to stronger, broader antibiotics. Those drugs cost more, cause more side effects, and increase the risk of dangerous infections like C. difficile and MRSA. The good news? You can find out for sure if you’re truly allergic-and most of the time, you’re not.
What a Real Penicillin Allergy Looks Like
A true penicillin allergy is an immune system reaction, not just a bad side effect. There are two main types: immediate and delayed.
Immediate reactions happen within an hour of taking the drug. These are the dangerous ones. Symptoms include hives, swelling of the lips or tongue, trouble breathing, a drop in blood pressure, or passing out. This is anaphylaxis-and it’s life-threatening. If you’ve ever had this, you need to be seen by an allergist.
Delayed reactions show up days later. The most common is a rash that appears 3 to 5 days after starting the antibiotic. It’s usually not dangerous, but it can be mistaken for something serious. Severe reactions like Stevens-Johnson Syndrome or DRESS are rare but require hospital care. If you had a rash that went away on its own after stopping the drug, it’s unlikely you’re truly allergic.
Why So Many People Get It Wrong
People often label themselves as allergic because:
- They got a rash as a child and were told it was penicillin
- They had nausea or diarrhea (common side effects, not allergies)
- They were told by a parent or a nurse decades ago
- They had a reaction to something else, like a virus, and blamed the antibiotic
Doctors used to err on the side of caution. But now we know that labeling someone as allergic without testing does more harm than good. Studies show that after 10 years without exposure, 80% of people who once had an IgE-mediated reaction lose their sensitivity. That means if you were told you were allergic 15 years ago, your risk today is probably near zero.
How to Find Out If You’re Really Allergic
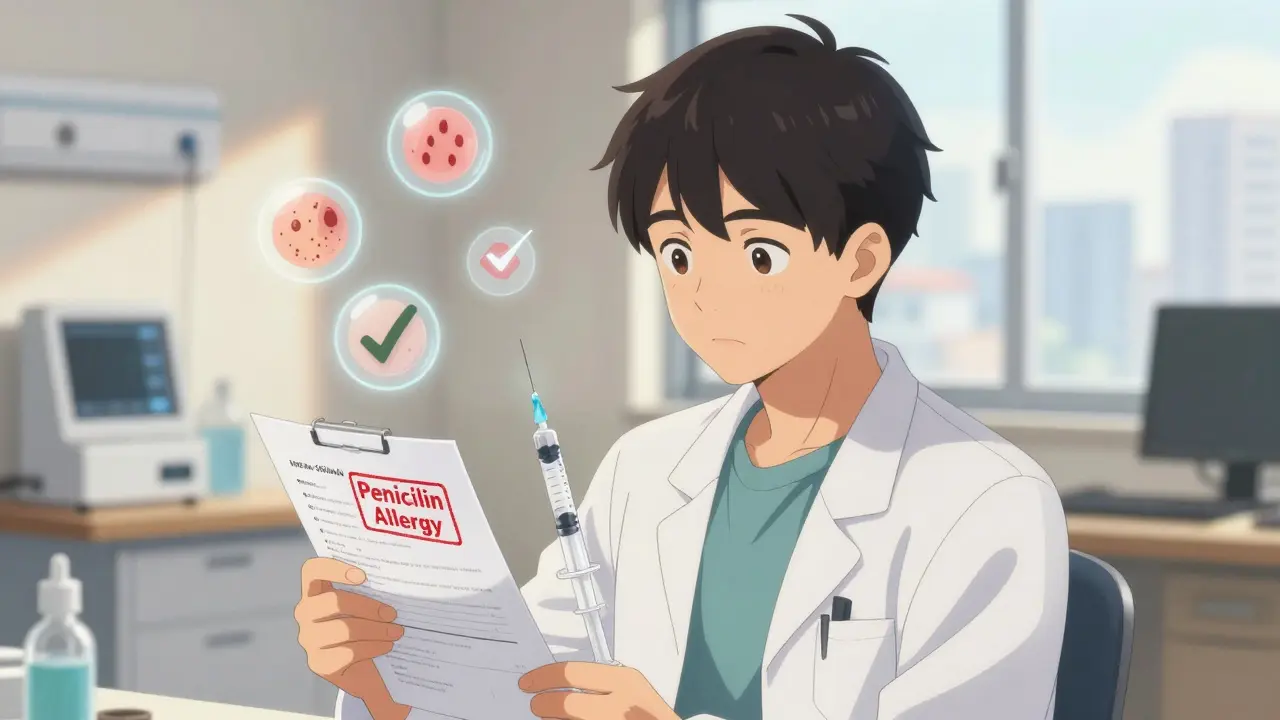
There’s a simple, safe way to test: skin testing followed by an oral challenge.
First, an allergist does a skin prick test using penicillin and its breakdown products. If that’s negative, they give you a small dose of amoxicillin-usually 250 mg-and watch you for an hour. No swelling? No itching? No trouble breathing? Then you’re not allergic.
This isn’t experimental. It’s standard practice in hospitals across the U.S. and the U.K. The CDC says that if both tests are negative, your risk of anaphylaxis drops to the same level as someone who’s never claimed an allergy. That’s not a guess-it’s backed by data.
And here’s the kicker: you don’t need to be terrified of the test. In over 20 years of clinical use, serious reactions during testing are extremely rare. The test is done in a controlled setting with emergency meds on hand. It’s safer than guessing.
What to Do If You’re Not Allergic
If testing clears you, you’re not just avoiding a label-you’re gaining access to better, cheaper, more effective antibiotics. Penicillin and amoxicillin are still the gold standard for treating strep throat, ear infections, pneumonia, and even some surgical infections.
After your test, make sure your doctor updates your medical record. Ask for a written note confirming you’re not allergic. If you’re going into surgery, tell your surgeon and anesthesiologist. Wear a medical alert bracelet only if you’ve had a true anaphylactic reaction. Otherwise, your medical record is your best protection.
What If You’re Actually Allergic?
If you’ve had a true anaphylactic reaction, or a severe skin reaction like SJS or TEN, you should avoid penicillin and related drugs (like ampicillin or amoxicillin) for life. But even then, you might not need to avoid all antibiotics.
Third- and fourth-generation cephalosporins (like ceftriaxone or cefdinir) and carbapenems (like meropenem) are generally safe for people without IgE-mediated symptoms. Many people who think they’re allergic to penicillin can take these without issue.
For those with confirmed IgE-mediated allergies, alternatives like clindamycin or vancomycin are used-but they’re not ideal. They’re more expensive, harder on the gut, and increase the chance of resistant infections. That’s why testing matters: it keeps you on the best drug, not just the safest one.
Why This Matters for Everyone
This isn’t just about you. Mislabeling penicillin allergies contributes to antibiotic resistance-a global crisis. Every time a doctor uses a broad-spectrum antibiotic because they think a patient is allergic, they’re helping superbugs evolve.
Studies show patients labeled as penicillin-allergic have a 50% higher chance of getting MRSA and a 35% higher chance of C. difficile. Hospitals that run formal penicillin de-labeling programs have reduced inappropriate antibiotic use by 20%. In orthopedic surgery, testing just 112 patients prevents one surgical infection.
The CDC estimates that fixing this one issue could save the U.S. healthcare system $1.2 billion a year. That’s not just money-it’s fewer hospital stays, fewer resistant infections, and fewer people dying from treatable conditions.
What You Should Do Right Now
Here’s what to do if you’ve ever said you’re allergic to penicillin:
- Check your medical records. Is it just listed as "penicillin allergy" with no details? That’s a red flag.
- Ask your doctor: "Was this confirmed with testing?" If not, ask if you’re a candidate for allergy evaluation.
- If you had a mild rash more than 5 years ago, or just stomach upset, you’re likely low-risk and can safely get tested.
- If you had swelling, trouble breathing, or anaphylaxis, see an allergist-even if it happened decades ago.
- Don’t assume your child’s reaction is permanent. Kids outgrow allergies more often than adults.
There’s no shame in being mislabeled. The system failed you by not testing. Now you have the power to fix it.
Penicillin Allergy Myths vs. Facts
| Myth | Fact |
|---|---|
| If I had a rash once, I’m always allergic. | Most rashes from penicillin are not allergic. Only 1 in 10 people with a rash are truly allergic. |
| Allergies last forever. | 80% of people lose sensitivity after 10 years without exposure. |
| Testing is dangerous. | Testing is safe and done under supervision. Reactions during testing are extremely rare. |
| I can’t take any antibiotics if I’m allergic to penicillin. | Many antibiotics, including ceftriaxone and azithromycin, are safe even if you’re allergic to penicillin. |
| Only kids get allergic reactions. | Reactions can happen at any age. But many people are mislabeled as children based on vague symptoms. |
Frequently Asked Questions
Can I outgrow a penicillin allergy?
Yes, most people do. About 80% of those with a true IgE-mediated reaction lose their sensitivity after 10 years without exposure. That’s why it’s important to get tested-even if you were told you were allergic as a child. Many adults who think they’re allergic have no reaction when properly tested.
Is penicillin allergy testing covered by insurance?
In most cases, yes. Allergy testing for penicillin is considered medically necessary by Medicare, Medicaid, and most private insurers. The cost is usually under $200, and it’s far less than the long-term costs of using broader antibiotics. Ask your doctor’s office to check your coverage before scheduling.
What if I need antibiotics right away and can’t wait for testing?
If you’re in an emergency and can’t wait, your doctor will choose an alternative antibiotic based on your reaction history. For low-risk patients (like those with only a past rash), cefazolin is often safe. For high-risk patients (like those with anaphylaxis), clindamycin or vancomycin may be used. But this is a temporary fix. Once you’re stable, get tested so you can use better antibiotics in the future.
Can I take amoxicillin if I’m allergic to penicillin?
Amoxicillin is part of the penicillin family. If you’re truly allergic to penicillin, you’re likely allergic to amoxicillin too. But here’s the key: most people who think they’re allergic to penicillin aren’t. If you’ve never been tested, you might safely take amoxicillin under supervision. A doctor can give you a small dose and watch you for an hour. If nothing happens, you’re not allergic.
Should I wear a medical alert bracelet for penicillin allergy?
Only if you’ve had a confirmed anaphylactic reaction or a severe skin reaction like Stevens-Johnson Syndrome. For most people who were labeled allergic as kids with a rash, a bracelet isn’t necessary-and it can cause harm by leading doctors to avoid the best antibiotics. Instead, make sure your allergy status is clearly documented in your electronic medical record and tell every provider you see.
Next Steps for Patients
If you’ve ever been told you’re allergic to penicillin, your next move is simple: call your primary care doctor and ask, "Can I be tested?" If they say no, ask for a referral to an allergist. Don’t wait until you’re in the hospital or facing surgery. Get it done now. You might be surprised at how safe and simple it is-and how much better your future care can be.





Posts Comments
henry mateo January 1, 2026 AT 00:24
i got labeled allergic to penicillin when i was 7 after a rash that lasted 3 days. never got tested. just assumed it was true. reading this made me realize how dumb that was. my doc never even asked if i wanted to get checked. kinda wild how many of us are just living with outdated labels.
Kunal Karakoti January 2, 2026 AT 04:15
the irony is that we fear the medicine meant to heal us, yet we accept the slow poison of broader antibiotics without question. penicillin isn’t the danger-it’s our collective ignorance dressed up as caution. evolution doesn’t care about our fears. it only rewards adaptation. maybe we should start adapting our medical thinking too.
Kelly Gerrard January 2, 2026 AT 18:08
if you think you have a penicillin allergy you need to get tested period. this isnt optional. its not a suggestion. its a public health emergency and you are part of the problem if you dont act. stop making excuses. your laziness is costing lives and billions. get it done now.
Shae Chapman January 3, 2026 AT 16:07
omg i just called my doctor and booked a test!! 🙌 i had a rash at 12 and thought i was doomed to avoid all antibiotics forever. turns out i probably never had a real allergy. i feel so relieved and kinda mad at my 12-year-old self for believing everything the nurse said 😅 thank you for this post!
Nadia Spira January 4, 2026 AT 08:26
this is the kind of performative medicine that makes me gag. you’re telling me we’re going to retest 100 million people because some lazy pediatrician mislabeled a kid in 1998? the system is broken. the answer isn’t more testing-it’s less trust in doctors who don’t even document properly. also ceftriaxone isn’t safe for everyone. don’t reduce complex immunology to a bullet point list.
Glendon Cone January 5, 2026 AT 07:47
i work in a hospital pharmacy and we’ve been pushing penicillin de-labeling for years. the best part? patients are usually shocked when they find out they’re not allergic. one guy cried because he’d avoided penicillin for 30 years and never knew he could’ve had a better, cheaper antibiotic for his pneumonia. it’s not magic. it’s just good science. everyone should get tested if they’ve ever said "i’m allergic" without proof.
Colin L January 7, 2026 AT 02:45
you know what’s really sad? not that people are mislabeled-it’s that we’ve turned medical care into a checklist culture. we don’t think anymore. we just click "allergy" because it’s easier than asking questions. and now we’re stuck with this bureaucratic mess where the only solution is more bureaucracy. i had a rash at 14, got labeled allergic, and now i’m 42 and still terrified of amoxicillin. i’ve never had a real reaction. but i’m too afraid to test. because what if they say yes? what if i’m still allergic? what if i die? what if i’m just… wrong? the system didn’t fail me. i failed myself by letting fear replace curiosity.
Hayley Ash January 7, 2026 AT 20:44
sure sure lets just retest everyone because apparently doctors are just idiots who can’t spell "allergy" correctly. next youll tell us we should retest everyone who says they're gluten intolerant. maybe the real issue is that people dont know the difference between side effects and allergies and now we're supposed to fix it with a $200 test? laughable. also why is no one talking about how often these "tests" are wrong? i bet half the people who test negative still react later. this is just medical theater
Henry Ward January 8, 2026 AT 21:18
if you're still alive after being mislabeled as allergic to penicillin for 20 years then you're not the victim here-you're the enabler. you let your fear become someone else's liability. you're not "just a patient"-you're part of a system that's killing people with unnecessary antibiotics. stop pretending you're innocent. you had the power to get tested. you chose not to. now you get to live with the consequences. and yes, i'm talking to you.
Write a comment