For many people with rheumatoid arthritis, remission isn’t a dream-it’s a real possibility. But getting there isn’t about hoping for the best. It’s about following a clear, science-backed plan called treat-to-target (T2T). This isn’t just another buzzword. It’s the standard of care recommended by top rheumatology groups worldwide, and it’s changing lives. If you’ve been told your RA is "under control" but you’re still tired, stiff, or in pain, you might not be on the right track. T2T flips the script: no more guesswork, no more waiting. It’s about hitting measurable goals-and staying there.
What Treat-to-Target Really Means
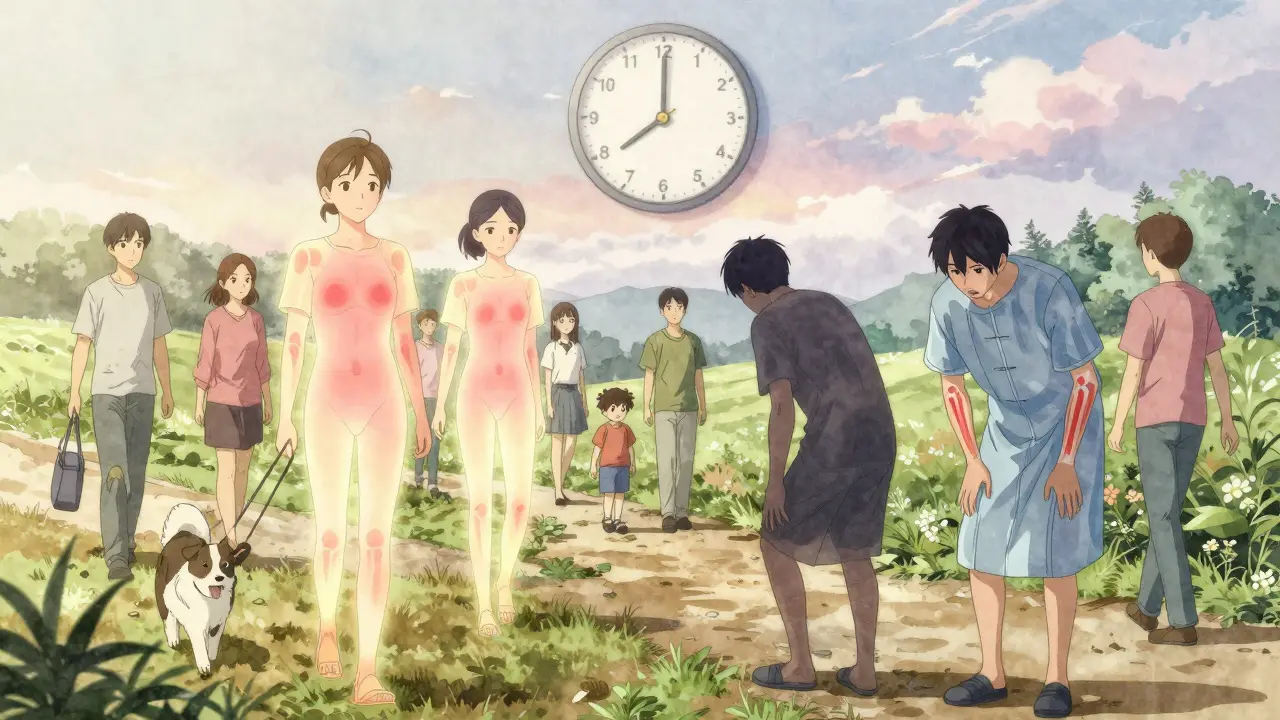
Treat-to-target isn’t a new drug or a fancy device. It’s a system. Think of it like managing diabetes or high blood pressure: you set a clear goal (like blood sugar under 7%), check your numbers regularly, and adjust your treatment if you’re not on track. For rheumatoid arthritis, the goal is either remission or low disease activity. Remission means no signs of active inflammation-no swollen joints, no morning stiffness, no elevated blood markers. Low disease activity means the inflammation is barely there, enough that you can live your life without it holding you back. The most common tool used to measure this is the DAS28 score. It counts 28 joints for swelling and tenderness, adds in a blood test (like CRP or ESR), and asks you how you’re feeling overall. A score below 2.6 is remission. Between 2.6 and 3.2? That’s low disease activity. Simple. Objective. Repeatable. And it’s checked every 1 to 3 months when your disease is active. No more waiting six months to see if a new drug "worked." If you’re not improving in 3 months, your treatment changes.Why This Works Better Than Old-School Care
Before T2T, many doctors adjusted treatment based on how they felt. If you seemed okay, they left things alone. If you complained, they might up the dose. But feelings aren’t data. And RA doesn’t wait. Left unchecked, even mild inflammation can slowly destroy your joints. Studies prove T2T works better. In the DREAM trial, 58% of people with early RA reached remission after a year using T2T. In routine care? Only 30%. The BeSt trial showed 61% remission with T2T versus 37% with standard care after two years. The TICORA trial found that even in people with longer-standing RA, T2T got more patients into low disease activity faster-and kept them there longer. The difference isn’t just numbers. People on T2T report better mobility, less pain, and higher quality of life. They’re more likely to keep working, playing with their kids, or hiking. And critically, joint damage slows or stops. X-rays show far less erosion over time. This isn’t just feeling better-it’s preventing permanent damage.How the Treatment Escalation Path Works
T2T isn’t just about measuring-it’s about acting. There’s a clear ladder of treatment options, and you move up if you’re not hitting your target. It usually starts with methotrexate. This is the foundation. Most people get 10-25 mg per week, often with folic acid to reduce side effects. If after 3 months your DAS28 is still above 3.2, you add another drug. That’s often triple therapy: methotrexate + sulfasalazine + hydroxychloroquine. It’s not glamorous, but it’s effective and affordable. If that doesn’t get you to remission within 6 months, you move to biologics or JAK inhibitors. Biologics like adalimumab, etanercept, or tocilizumab block specific parts of the immune system that drive inflammation. JAK inhibitors like baricitinib or upadacitinib work inside cells to stop the same signals. These drugs are powerful. They can turn things around-even when other treatments failed. The key is timing. Every 3 months, you reassess. No delays. No "let’s wait and see." If you’re not improving, you escalate. This aggressive, early approach is what makes T2T so effective.
Real-World Gaps: Why It’s Not Working Everywhere
Here’s the problem: not everyone is getting this care. A 2022 study found that while nearly 80% of rheumatologists say they aim for remission, only 41% actually set a clear goal with their patients. That’s a huge gap. Some doctors still rely on old habits. They check CRP once a year. They don’t count joints properly. They wait too long to switch meds. Patients often don’t know what remission means. They think "feeling okay" is good enough. But remission isn’t about feeling okay-it’s about having no detectable inflammation. One patient on a forum wrote: "My doctor says I’m doing well. But I’m still swollen. I asked for a DAS28. He said we don’t need it." That’s not T2T. That’s business as usual. Another issue: access. Biologics and JAK inhibitors are expensive. In the UK, NHS access can vary by region. In low-income countries, many can’t even get methotrexate regularly. That’s why global adoption is only 25% in some areas.What You Can Do to Make T2T Work for You
If you have RA, you’re not powerless. Here’s how to take charge:- Ask your rheumatologist: "What’s my DAS28 score?" If they don’t know or don’t track it, ask why.
- Request a written treatment plan with your target: remission or low disease activity.
- Track your own symptoms between visits. Use a journal or app. Note joint pain, stiffness, fatigue.
- Ask: "If I’m not at target in 3 months, what’s the next step?" Know the plan before you start.
- Don’t stop meds because you feel better. Remission doesn’t mean cure. Stopping treatment often leads to flare-ups.
What If You Can’t Reach Remission?
Not everyone gets to remission. That doesn’t mean you’ve failed. The 2022 EULAR guidelines now say: if remission isn’t possible, aim for low disease activity-and focus on your quality of life. Maybe you can’t jog anymore, but you can play with your grandkids. Maybe you need a cane, but you’re working full-time. Those are wins. Dr. Paul Emery from the University of Leeds reminds us: "The goal isn’t just to hit a number. It’s to help you live the life you want." Sometimes, that means accepting a little inflammation to avoid harsh side effects. Sometimes, it means switching from a biologic to a cheaper drug that still keeps you functional. T2T isn’t about perfection. It’s about progress. And progress is measured in real life-not just scores.What’s Next for T2T?
The future is getting smarter. Trials are testing digital tools-smartphone apps that let you log pain, swelling, and fatigue daily. These feed into your doctor’s system and flag changes before you even walk in. One trial, called DART, is testing whether this can cut visits in half while improving outcomes. Another big shift: personalized treatment. Researchers are studying genes, proteins, and immune markers to predict who will respond to which drug. Soon, you might get a blood test that says: "You’re likely to respond well to tocilizumab, not adalimumab." That’s the next leap-T2T, but tailored to your biology. For now, the best thing you can do is start where you are. Ask for your score. Know your target. Stick to the plan. Remission is possible. But only if you and your doctor are working together-with clear goals, regular checks, and the courage to change course when needed.What does remission mean in rheumatoid arthritis?
Remission in rheumatoid arthritis means there’s no detectable sign of active inflammation. This is measured using tools like DAS28, where a score below 2.6 indicates remission. You won’t have swollen or tender joints, normal blood markers like CRP or ESR, and minimal or no morning stiffness. It doesn’t mean the disease is gone-it means it’s under control enough that joint damage stops and daily life isn’t limited.
How often should DAS28 be checked in RA treatment?
During active disease, DAS28 should be checked every 1 to 3 months. This is key to the treat-to-target approach-treatment adjustments happen if targets aren’t met within 3 months. Once you reach stable remission or low disease activity, checks can be reduced to every 3 to 6 months. Consistent monitoring is what makes T2T effective, not just the medications.
What are the first-line drugs in treat-to-target for RA?
Methotrexate is the first-line drug in most treat-to-target protocols. It’s usually started at 10-25 mg per week, often with folic acid. If it’s not enough after 3 months, doctors typically add a second or third conventional DMARD-like sulfasalazine and hydroxychloroquine-in what’s called triple therapy. Only if these don’t work after 6 months do they move to biologics or JAK inhibitors.
Can you reach remission with established RA?
Yes, but it’s harder. Studies show people with early RA (less than a year of symptoms) have the best chance-up to 60% can reach remission with T2T. In established RA (more than 2 years), remission rates drop, but many still reach low disease activity. The TICORA trial showed even in long-standing RA, T2T got more patients into low disease activity faster than routine care. The goal shifts from full remission to minimizing symptoms and preventing further damage.
Why do some doctors not use treat-to-target?
Several reasons: time constraints, lack of training in joint counting or scoring tools, limited access to biologics, and resistance to change. A 2020 ACR survey found only 58% of rheumatologists use standardized disease activity scores at every visit. Some still rely on how patients "look" or feel. Others worry about the cost of biologics or fear pushing patients too hard. Patient reluctance also plays a role-some don’t want frequent visits or blood tests. But when implemented well, T2T leads to better outcomes.







Posts Comments
Julie Chavassieux December 21, 2025 AT 21:51
Remission? More like a fairy tale they sell you so you stop complaining.
Kathryn Weymouth December 23, 2025 AT 14:40
I’ve been on methotrexate for 4 years. My DAS28 was 4.1 last month. My rheumatologist said I’m "doing fine." I asked for a printout. He looked confused. This isn’t care-it’s negligence dressed in white coats. I’m switching doctors.
Cara Hritz December 24, 2025 AT 08:05
why do they even use das28? i heard its outdated and theyre moving to cliq scores now? or is that just for psoriatic? i think i read somethin bout it on reddit but i cant find the thread anymore lol
Jamison Kissh December 24, 2025 AT 23:05
There’s something deeply human about this whole framework. We treat RA like a broken machine that needs tuning-but it’s not. It’s a living system, a silent rebellion inside the body. The T2T model tries to impose order on chaos, but what if the chaos is the body’s last honest voice? Maybe remission isn’t the goal. Maybe it’s harmony. Maybe we’re not supposed to silence inflammation-we’re supposed to listen to why it’s there.
Sam Black December 25, 2025 AT 17:55
As someone who’s been in remission for 3 years on methotrexate + folic acid, I just want to say: this post saved my life. I used to think "feeling okay" was enough. Then I learned what remission really meant. No more 6 a.m. stiffness. No more hiding my swollen knuckles. I started hiking again. I’m not cured-but I’m alive. And if you’re reading this and your doctor won’t check your DAS28? Bring this article. Print it. Slide it across the table. You deserve better.
Kiranjit Kaur December 26, 2025 AT 02:30
OMG YES!! 🙌 I’m from India and we don’t even have access to biologics in my town. My doc put me on triple therapy and I cried when my DAS28 dropped to 2.4. It’s not perfect, but it’s progress. 💪 Don’t let anyone tell you remission is only for rich countries. We’re fighting too. #RAWarrior
Art Van Gelder December 27, 2025 AT 08:41
Let me tell you about my cousin’s friend’s neighbor’s rheumatologist in Ohio-this guy, he’s like a medieval alchemist. He believes in "energy balancing" and only sees patients every six months. One time, he told my cousin, "Your joints look less red today, so you’re probably fine." My cousin had a DAS28 of 5.8. Five point eight. And this guy was nodding like he’d just cured cancer. I swear, if I didn’t find this article, I’d still be wondering why I can’t open a jar of pickles. The system is broken. But knowledge? Knowledge is the scalpel.
Candy Cotton December 28, 2025 AT 09:24
It is an incontrovertible fact that the Treat-to-Target paradigm represents the pinnacle of evidence-based rheumatological practice, as codified by the American College of Rheumatology, the European League Against Rheumatism, and the International Society for Rheumatology. Any deviation from this protocol constitutes a dereliction of professional duty, particularly in a nation as scientifically advanced as the United States. The notion that access to biologics should be contingent upon geography or socioeconomic status is not merely inefficient-it is morally indefensible. We must demand systemic reform. Now.
Johnnie R. Bailey December 29, 2025 AT 18:26
One thing nobody talks about: the emotional toll of chasing remission. You’re told to be aggressive, to escalate, to not settle. But what if you’re tired? What if you’ve lost your job, your insurance, your will to fight? T2T doesn’t account for burnout. I hit remission once-then stopped meds because I couldn’t afford the copay. Flared in 3 weeks. Now I’m back on it. I’m not a statistic. I’m a person. And sometimes, the goal isn’t to hit 2.6-it’s to just get through the day without crying. That’s still worth honoring.
Vikrant Sura December 31, 2025 AT 03:36
Why are we even talking about this? Biologics cost $20k a year. Who cares if you hit a score? You’re still gonna die in 10 years. This is just pharma’s way of selling more drugs. Stop chasing numbers. Start chasing peace.
Sai Keerthan Reddy Proddatoori December 31, 2025 AT 11:44
They want you to take these drugs because the government is controlling your immune system. The DAS28? Fake metric. CRP? Manufactured. They don’t want you healed-they want you dependent. I stopped all meds. Now I drink turmeric tea and sleep on copper mats. My joints feel better. The system hates free people.
Jeremy Hendriks January 1, 2026 AT 16:57
Remission is a capitalist illusion. You’re not supposed to feel better-you’re supposed to keep working, keep consuming, keep paying for your meds. The real target isn’t your DAS28 score. It’s your wallet. They want you addicted to the system, not cured. I’ve seen it. I’ve been there. You think you’re winning? You’re just another cog.
Herman Rousseau January 2, 2026 AT 13:34
Hey everyone-just wanted to say thank you to the person who wrote this. I showed it to my doc last week. She actually printed out a copy for me. We set my target: DAS28 under 3.2 by next month. I’ve been tracking my pain with an app now. I’m not fixed-but I’m finally being heard. And that? That’s everything. 💙
Write a comment