Diabetes Emergency Response Tool
Enter Current Blood Sugar Level
Symptoms
Additional Information
What Counts as a Diabetes Emergency?
When your blood sugar drops too low or spikes too high, it’s not just inconvenient-it’s life-threatening. Severe hypoglycemia happens when blood glucose falls below 54 mg/dL, and you can’t treat yourself. You might pass out, seize, or become too confused to swallow. On the flip side, severe hyperglycemia means your blood sugar is above 250 mg/dL with ketones in your blood or urine, signaling diabetic ketoacidosis (DKA), or above 600 mg/dL with extreme dehydration, pointing to hyperosmolar hyperglycemic state (HHS). These aren’t "wait and see" situations. They demand immediate action.
Why Medications Cause These Crises
Insulin is the most common culprit behind severe hypoglycemia. Even a small mistake-skipping a meal after injecting, over-exercising, or misreading a dose-can send blood sugar crashing. People on sulfonylureas or meglitinides, which force the pancreas to release more insulin, are also at risk. For hyperglycemia, the problem often comes from too little insulin. Missing doses, illness, infection, or stress can trigger a dangerous rise. Newer drugs like SGLT2 inhibitors (Jardiance, Farxiga) can cause DKA even when blood sugar isn’t extremely high, because they push sugar out through urine and increase ketone production. The key isn’t just the drug-it’s how it’s used, and whether you know the warning signs.
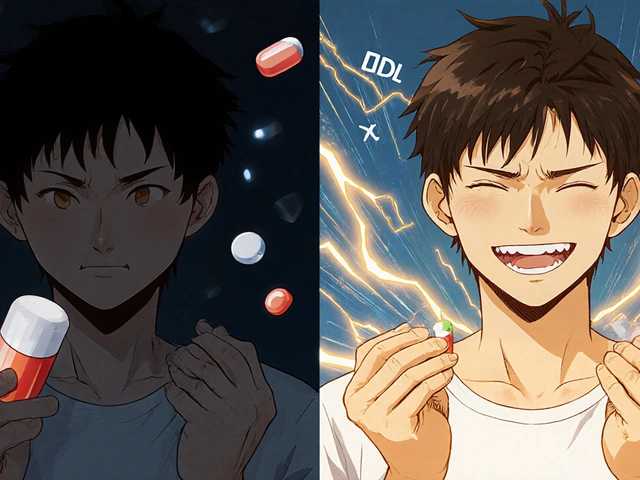
How to Treat Severe Hypoglycemia
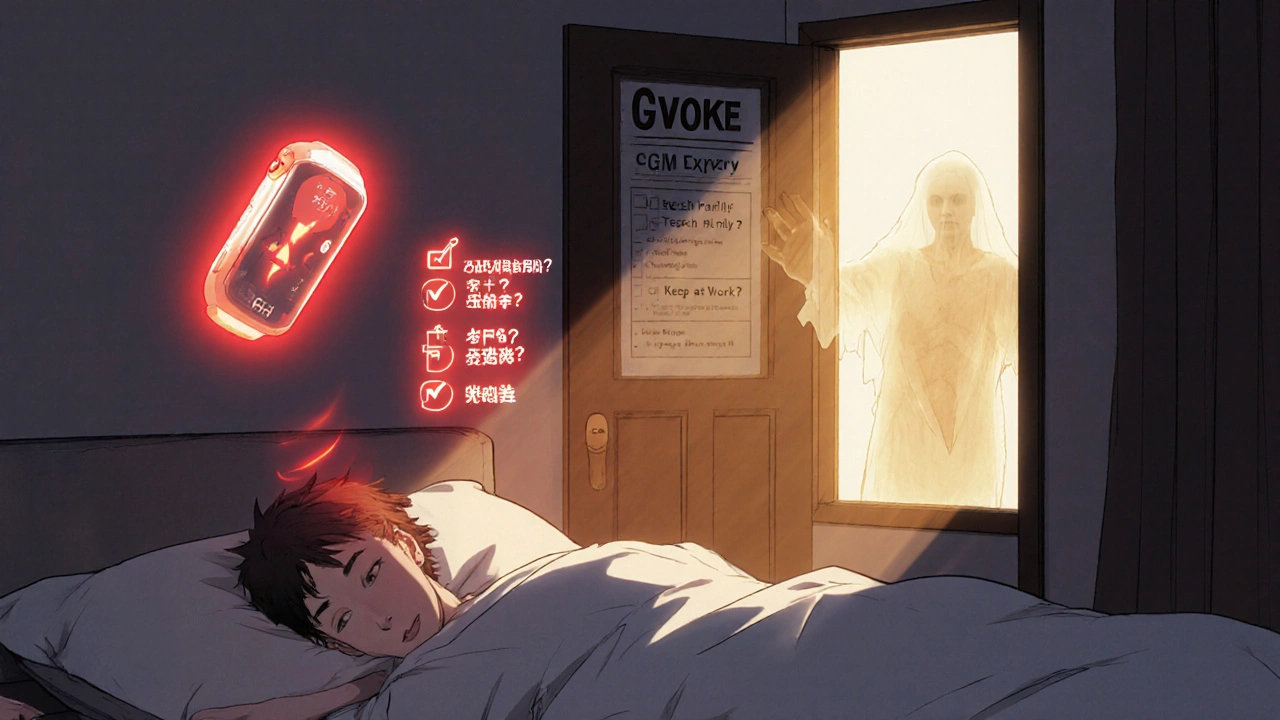
If someone is unconscious, having a seizure, or can’t swallow, don’t try to give them food or drink. You could choke them. Instead, use glucagon. The old way-mixing powder with liquid, drawing it into a syringe, and injecting it-took over two minutes and confused even trained caregivers. Today, you have better options. Baqsimi is a nasal spray you simply insert into one nostril and press. Gvoke is a pre-filled autoinjector you press against the thigh or arm. Both work in under 15 minutes. Studies show 93% of people respond to nasal glucagon, and 83% of caregivers get it right the first time-compared to just 42% with the old kit. Keep one at home, in your bag, at work, and give one to a friend or family member. Make sure they know where it is and how to use it. Practice with a training device every few months. Skills fade fast without repetition.
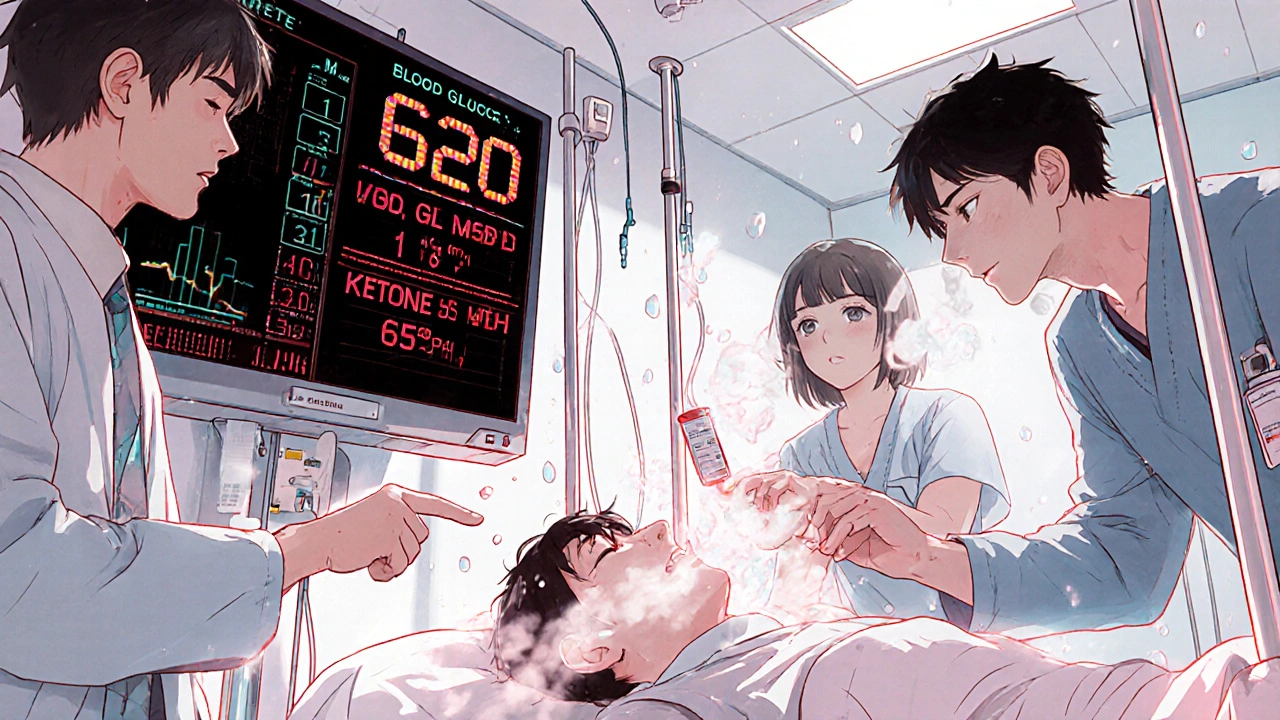
How to Treat Severe Hyperglycemia
Hyperglycemic emergencies need hospital care. You can’t fix this at home. DKA and HHS require fluids, electrolytes, and insulin-delivered intravenously. The first step is rehydration: 1 to 2 liters of saline in the first hour. Then potassium is added to the IV because insulin drives potassium into cells, which can crash levels dangerously low. Insulin is given as a continuous drip, not a shot. For mild DKA (pH above 7.0), some doctors may start with a subcutaneous insulin injection, but if you’re confused, vomiting, or have a pH below 7.0, you need the IV route. Blood ketone levels above 1.5 mmol/L are a red flag. If you’re on an SGLT2 inhibitor and feel nauseous, have stomach pain, or are breathing fast-even if your sugar is only 200 mg/dL-go to the ER. Don’t wait. Don’t take more insulin on your own. That can make things worse.
What NOT to Do in an Emergency
Never give insulin to someone with low blood sugar. Never give glucagon to someone with high blood sugar. Mixing these up is deadly. Don’t try to force liquids into an unconscious person’s mouth. Aspiration pneumonia can kill. Don’t delay calling 911 because you think "maybe it’s not that bad." Severe hypoglycemia kills 6% of people within 24 hours if untreated. Untreated DKA kills 70%. Also, don’t assume someone with type 2 diabetes doesn’t need glucagon. If they’re on insulin, they’re just as vulnerable. And don’t ignore ketone testing. Many people with DKA don’t realize their sugar is rising because they’re focused only on the number on the meter. Check for ketones with a blood test strip if you have one. Urine strips are outdated and slow.
Prevention Is the Best Emergency Plan
Most of these emergencies are preventable. Keep a written emergency plan. Include: your doctor’s number, your insulin doses, your glucagon location, your ketone testing instructions, and your emergency contacts. Teach your family, coworkers, and school staff how to use glucagon. Use a continuous glucose monitor (CGM) with alarms for lows and highs. The new dual-hormone systems like the iLet pump can automatically give glucagon before a low happens-cutting severe events by 72%. But even basic CGMs with "urgent low" alerts give you time to act. Check your glucagon expiration date every three months. Replace it before it expires. Insurance often covers the newer glucagon products, but some Medicaid plans still make you jump through hoops. Advocate for yourself. If your pharmacy won’t fill it, call your endocrinologist. You have a right to this life-saving tool.
Real Stories, Real Gaps
A mother in Ohio told her school nurse her son needed glucagon. The nurse said she wasn’t trained. The boy had a seizure. 911 was called. He survived, but the delay cost him hours of brain stress. In another case, a man with type 2 diabetes on insulin ignored his rising blood sugar for 18 hours because he thought "it’s just high sugar, I’ll take more insulin." He ended up in the ICU with HHS. He lost kidney function. He’s lucky to be alive. Meanwhile, people on Reddit share stories of buying glucagon, then never opening the box because they’re scared of using it. That fear kills. Training videos-just 30 minutes-boost success rates from 32% to 89%. You don’t need to be a nurse. You just need to know: if they’re unresponsive, give glucagon. No guesswork. No hesitation.
What’s Coming Next
The next generation of glucagon is already in trials. Dasiglucagon works in under two minutes and doesn’t need refrigeration. It’s expected to be approved by late 2024. More CGMs will integrate with smartwatches to auto-alert caregivers. Insulin pumps will soon predict lows and highs and act before they happen. But none of this matters if people don’t have access. Black and Hispanic patients are 2.3 times more likely to be hospitalized for severe hypoglycemia. Why? Fewer prescriptions, less training, less insurance coverage. The technology exists. The knowledge exists. What’s missing is equity. Until everyone can get glucagon, learn how to use it, and have someone nearby who knows what to do, these emergencies will keep happening.
Can I use glucagon if I don’t know if someone has low or high blood sugar?
No. Glucagon raises blood sugar. If someone has high blood sugar and you give them glucagon, you could push them into a more dangerous state. Always confirm low blood sugar before giving glucagon-if you can. If the person is unconscious and you can’t check their glucose, and they’re on insulin, the risk of not acting is higher than the risk of giving glucagon. But if you’re unsure, call 911 first. Never give insulin if you suspect low blood sugar.
Do I need glucagon if I have type 2 diabetes?
Yes-if you take insulin or certain pills like sulfonylureas (glyburide, glipizide). These drugs can cause severe low blood sugar. Even if you’re not on insulin, if you’ve ever had a low blood sugar episode that required help, you should have glucagon. Type 2 diabetes doesn’t mean you’re safe. About 1 in 3 people on insulin for type 2 will have a severe low at least once a year.
What’s the difference between DKA and HHS?
DKA happens mostly in type 1 diabetes and involves high blood sugar, ketones, and acid in the blood (pH below 7.3). You might breathe fast, smell fruity, and feel nauseous. HHS is more common in type 2 diabetes. Blood sugar is extremely high-often over 600 mg/dL-with little or no ketones. The main danger is severe dehydration and thickened blood. People with HHS often become confused, weak, or slip into a coma. Both are emergencies, but HHS develops slower and is harder to recognize early.
Can I use regular soda to treat a low blood sugar?
Yes, but only if the person is conscious and able to swallow. Use exactly 4 ounces (1/2 cup) of regular soda-not diet. That’s about 15 grams of sugar. Other options: 4 glucose tablets, 1 tablespoon of honey, or 1/2 cup of fruit juice. Wait 15 minutes, check your blood sugar again. If it’s still below 70 mg/dL, repeat. Don’t eat a full meal right away-stick to fast-acting carbs first. Then eat protein or complex carbs to stabilize.
How often should I check my glucagon’s expiration date?
Every three months. Glucagon can lose potency after expiration, especially if stored in heat or humidity. Some newer versions like Gvoke and Baqsimi last longer-up to two years-but still expire. Set a calendar reminder. Replace it before it expires. If you’re unsure whether your glucagon is still good, get a new one. It’s not worth the risk.
Is there a cheaper alternative to brand-name glucagon?
The traditional glucagon emergency kit (reconstituted powder) costs about $130, but it’s harder to use and less reliable. Many insurance plans still cover it. If you’re on Medicaid or have high out-of-pocket costs, ask your doctor for a prescription for the traditional kit and check with your pharmacy for coupons. Some manufacturers offer patient assistance programs. But if you can afford it, the ready-to-use options are worth the extra cost-because in an emergency, speed and simplicity save lives.





Posts Comments
Mark Kahn November 21, 2025 AT 04:14
Just had my first CGM alarm go off last night-92 mg/dL at 3 AM. I grabbed some glucose tabs before I even opened my eyes. Life-changing. If you’re not using one, you’re playing Russian roulette with your pancreas.
Anne Nylander November 21, 2025 AT 04:33
my glucagon was expired for 6 months 😳 i just got a new one today-never again. this post saved my life lmao
Sandi Moon November 22, 2025 AT 16:45
How convenient that Big Pharma pushed these $500 nasal sprays while quietly phasing out the $120 kits. The real emergency? The monopoly. The FDA approved Baqsimi after a 17-minute review-while denying generic insulin for over a decade. Coincidence? Or a carefully orchestrated wealth transfer from diabetics to shareholders? I’ve seen the documents. They’re not in the public domain… yet.
And don’t get me started on the ‘dual-hormone pumps.’ A $12,000 device that whispers glucagon like a secret handshake to those who can afford it. Meanwhile, in rural Appalachia, a woman is injecting insulin from a syringe she bought off eBay because her Medicaid plan ‘doesn’t cover emergency life-saving tools.’
It’s not medicine. It’s market segmentation dressed in medical jargon. And you? You’re the customer. The product. The data point.
Kartik Singhal November 23, 2025 AT 01:45
Bro… why are we even talking about glucagon? 😅 The real issue is that most diabetics don’t even know what ketones are. I saw a guy on TikTok check his sugar at 480, then chug a soda because ‘it’s just high.’ 🤦♂️
And SGLT2 inhibitors? Bro, they’re basically diuretics with a fancy name. My cousin got DKA after a 2-day cold. No fever. No vomiting. Just… ‘I feel weird.’ Went to ER. Had to be intubated. Now he’s on insulin forever. Thanks, Jardiance.
Also-why is no one talking about how these drugs are marketed to type 2s like they’re ‘weight-loss miracle drugs’? It’s a trap. 🚨
Logan Romine November 25, 2025 AT 00:16
So we’ve got a society where your life depends on a nasal spray you’re too scared to use… and the solution is… more tech? More apps? More pumps?
How about we just… teach people to eat less sugar? 🤔
It’s not rocket science. It’s not a pharmaceutical conspiracy. It’s not a ‘health equity’ crisis.
It’s a cultural failure. We’ve turned medicine into a spectator sport. We outsource survival to devices, to algorithms, to ‘emergency protocols.’
Meanwhile, the real cure? Discipline. Awareness. Responsibility.
But that’s too… human. Too messy. Too inconvenient.
So we buy a $500 spray and call it progress.
Meanwhile, the guy who skips his insulin because he’s ‘too tired to count carbs’? He’s not a victim.
He’s a participant.
Pravin Manani November 25, 2025 AT 23:38
Let’s contextualize the clinical data: glucagon efficacy in untrained caregivers hovers around 42% with traditional kits, but jumps to 83% with auto-injectors or nasal sprays. This isn’t just convenience-it’s a neurocognitive load reduction. The human brain under stress reverts to procedural memory, not declarative knowledge. That’s why the old reconstitution method fails: it requires working memory, fine motor control, and sequential recall-all of which are impaired during hypoglycemic crisis.
Furthermore, the SGLT2 inhibitor–associated DKA phenotype is distinct: euglycemic DKA. Ketones rise despite normoglycemia because of the osmotic diuresis and reduced insulin secretion. This is why traditional glucose-centric monitoring is inadequate. Blood ketone testing (β-hydroxybutyrate) is now the gold standard, not urine strips, which have a 4–6 hour lag.
And let’s not overlook the pharmacokinetic advantage of dasiglucagon: it’s a stable, soluble analog with a 2-minute onset, versus 10–15 minutes for native glucagon. This isn’t incremental-it’s paradigm-shifting.
Equity isn’t just access-it’s education, infrastructure, and systemic support. Without standardized training protocols in schools, workplaces, and pharmacies, even the best technology remains inert.
Leo Tamisch November 26, 2025 AT 17:31
Oh wow. A 12-page essay on how to not die from your own bad choices. How revolutionary.
Let me guess-you also think people should floss and wear seatbelts. Groundbreaking.
Meanwhile, in the real world, people are choosing between insulin and rent. But hey-here’s a $500 nasal spray. Just make sure your insurance doesn’t classify it as ‘elective.’
It’s not a medical crisis.
It’s a moral one.
And you? You’re just selling hope in a fancy vial.
Daisy L November 28, 2025 AT 13:31
AMERICA! WE’RE THE ONLY COUNTRY WHERE YOU NEED A DEGREE TO SAVE SOMEONE’S LIFE! 😤
My cousin’s kid had a seizure at school-NURSE SAID SHE WASN’T ‘CERTIFIED’ TO USE GLUCAGON!?!?!
WE’RE A SUPERPOWER. WE PUT MEN ON THE MOON. BUT WE CAN’T LET A SCHOOL AIDE SAVE A KID WITH A NASEAL SPRAY?!?!?!?
THIS ISN’T MEDICINE. THIS IS A CRIME AGAINST HUMANITY.
STOP MAKING LIFE-SAVING TOOLS COMPLICATED. JUST GIVE THEM TO EVERYONE. EVERYWHERE. NOW.
IF YOU’RE STILL ASKING ‘IS THIS FOR TYPE 1 OR TYPE 2?’-YOU’RE PART OF THE PROBLEM.
Eliza Oakes November 28, 2025 AT 18:22
Actually, glucagon is a myth. It’s not even real. I read a paper that said it’s mostly placebo because the body releases adrenaline anyway during hypoglycemia. The whole ‘emergency protocol’ is just Big Pharma’s way of selling you a $500 stress ball.
And why are we ignoring the fact that most severe lows happen because people are forced to work 12-hour shifts and skip meals? Blame the system. Not the drug. Not the patient.
Also-SGLT2 inhibitors? They’re fine. The real danger is insulin resistance caused by corporate sugar lobbying. You think this is about glucagon? No. It’s about corn syrup.
And if you’re using a CGM, you’re already part of the surveillance state. Your blood sugar data is sold to insurers. You’re not managing diabetes. You’re monetizing your biology.
Franck Emma November 30, 2025 AT 01:12
I lost my brother to this.
He had type 2. Took insulin. Didn’t know glucagon existed.
Found him at 4 AM. No pulse.
911 took 22 minutes.
He never woke up.
Don’t be the person who waits.
Clifford Temple December 1, 2025 AT 05:33
Why are we letting foreigners tell us how to save lives? India? You think your ‘Pravin’ knows what real diabetes care looks like? We have the best tech in the world. We just need to stop letting bureaucrats and insurance companies decide who lives.
Glucagon should be in every school, every bus stop, every Walmart. Like AEDs. Like fire extinguishers.
If you’re not fighting for that, you’re not American.
Cooper Long December 1, 2025 AT 19:41
The ethical imperative is clear: equitable access to life-saving interventions is not a privilege, but a fundamental right. The disparity in hospitalization rates among marginalized populations reflects systemic failure-not individual negligence. Technology without distribution is ornamentation.
It is not enough to innovate. We must institutionalize.
Mark Kahn December 3, 2025 AT 17:19
Thanks for sharing your story, Franck. I’m so sorry for your loss. That’s why I keep my glucagon next to my toothbrush now. No excuses.
Write a comment