HAS-BLED Bleeding Risk Calculator
Assess Your Bleeding Risk
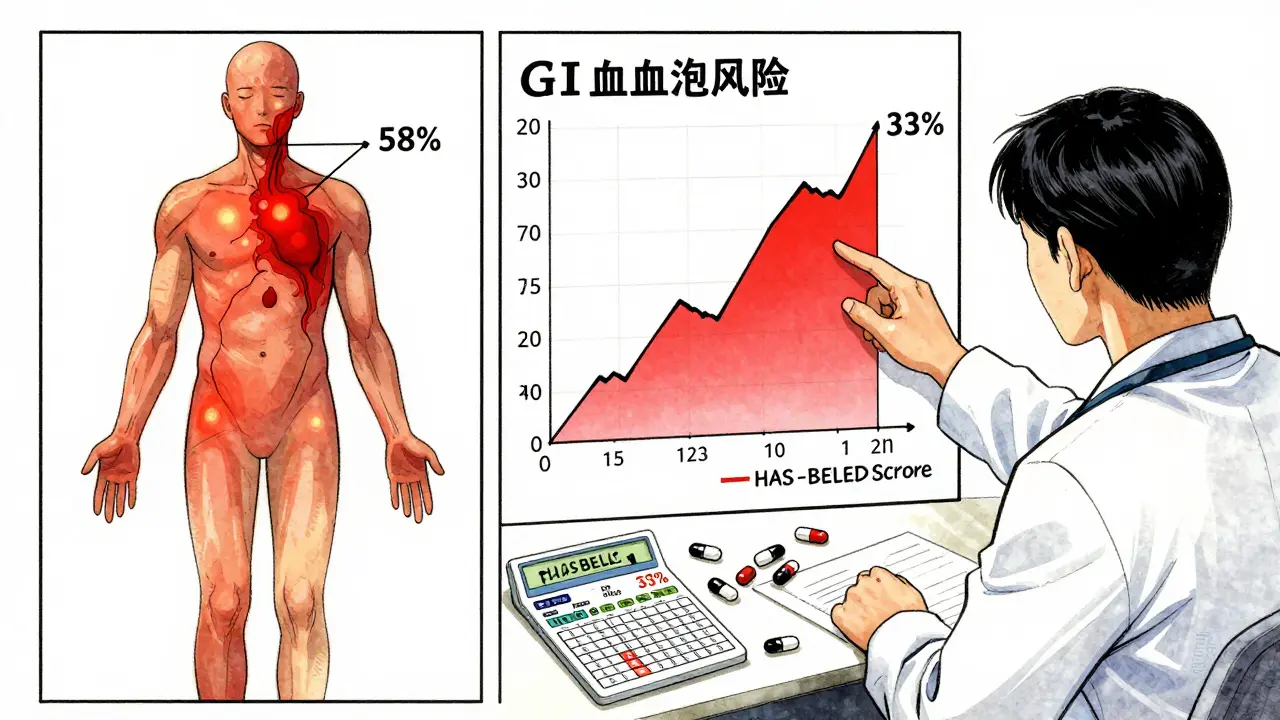
This tool calculates your HAS-BLED score, a clinical tool used to assess bleeding risk when taking SSRIs with anticoagulants. The article shows that combining these medications increases bleeding risk by 33%.
Your HAS-BLED Score
When you’re on blood thinners like warfarin or apixaban, you’re already managing a delicate balance. Now add an SSRI-like sertraline or escitalopram-for depression or anxiety, and suddenly the risk of bleeding goes up. Not by a little. Not by guesswork. By 33%. That’s not a theoretical concern. It’s a real, measurable, and well-documented danger backed by data from over 42,000 patients in a 2024 study published in JAMA Network Open.
Why SSRIs Make Blood Thinners More Dangerous
SSRIs don’t thin your blood the way aspirin or warfarin does. Instead, they mess with your platelets-the tiny blood cells that rush to seal cuts and prevent bleeding. Platelets need serotonin to stick together and form clots. SSRIs block the serotonin transporter on platelets, which means serotonin gets sucked out of them and can’t do its job. At therapeutic doses, this cuts platelet serotonin uptake by up to 90%. The result? Platelets can’t aggregate properly. Your body’s first line of defense against bleeding weakens.This isn’t new science. Researchers first linked SSRIs to platelet dysfunction in the early 2000s. But what changed in 2024 was the scale of the evidence. The study tracked nearly 1.2 million people with atrial fibrillation-many on anticoagulants-and found those taking SSRIs had a 33% higher chance of major bleeding compared to those on anticoagulants alone. That’s 6 extra bleeding events per 1,000 patients each year. For someone already at risk, that’s significant.
Where the Bleeding Happens
Bleeding isn’t random. It shows up in predictable places:- Gastrointestinal bleeding makes up 58% of cases. This includes stomach ulcers, intestinal bleeding, or even bleeding from the rectum. It’s the most common and often the most dangerous because it can be slow and hidden.
- Intracranial hemorrhage (bleeding in the brain) accounts for 17%. Even a small bleed here can be life-changing or fatal.
- The remaining 25% are other major bleeds-like muscle, joint, or internal organ bleeds.
The absolute risk goes from 1.8 bleeding events per 100 person-years on anticoagulants alone to 2.4 when you add an SSRI. That might sound small, but when you’re talking about hundreds of thousands of patients on these drugs, it adds up fast. In the U.S. alone, this interaction could be costing over $1.2 billion annually in avoidable hospitalizations.
Not All Blood Thinners Are the Same
You might assume all anticoagulants behave the same with SSRIs. They don’t.Traditional warfarin (a vitamin K antagonist) carries a higher risk when combined with SSRIs-about a 28% increase in bleeding. Direct oral anticoagulants (DOACs) like rivaroxaban, apixaban, or dabigatran show a slightly lower risk-around 22%. But here’s the catch: that difference wasn’t statistically significant. So while DOACs may be safer, you can’t assume they’re safe enough to ignore the risk.
Warfarin requires regular INR blood tests. When you add an SSRI, your doctor might need to check your INR twice a week for the first month. DOACs don’t need routine monitoring, but that doesn’t mean they’re risk-free. The platelet effect from SSRIs still applies.
Not All SSRIs Are Equal-But Not for the Reason You Think
You might think the strongest SSRI-like paroxetine-would cause the most bleeding. After all, it’s the most potent at blocking serotonin reuptake. But the 2024 study found no difference in bleeding risk between paroxetine, sertraline, escitalopram, or fluoxetine. Even though escitalopram is weaker at blocking serotonin, it carried the same risk. That’s surprising. It means the risk isn’t about how strong the drug is-it’s about whether it’s an SSRI at all.Earlier studies, like one from 2018, suggested rivaroxaban might be safer with SSRIs than warfarin. But the newer, larger data shows that while DOACs may have a slight edge, the difference isn’t big enough to change clinical practice. The real takeaway? Any SSRI + any anticoagulant = increased bleeding risk.
Who’s at Highest Risk?
Not everyone on this combo will bleed. But some people are much more vulnerable:- People with a HAS-BLED score of 3 or higher-that’s a tool doctors use to measure bleeding risk based on things like high blood pressure, kidney disease, previous bleeding, and age.
- Those over 75.
- People with a history of ulcers or GI bleeding.
- Anyone taking NSAIDs like ibuprofen or naproxen on top of their anticoagulant and SSRI.
- Patients in the first 30 days of starting the combo. That’s when the risk peaks.
After six months, the risk drops significantly. That’s likely because the body adapts, or doctors become more cautious with monitoring. But those first few weeks? That’s when you need to be extra careful.

What Doctors Are Doing About It
In 2017, the American Heart Association warned about this interaction. In 2019, the FDA added bleeding warnings to SSRI labels after reviewing 27 serious case reports. In 2025, the FDA updated medication guides again-this time urging doctors to consider non-SSRI antidepressants for patients with extra bleeding risks.Guidelines now recommend:
- Checking CBC and fecal occult blood tests at baseline and monthly for the first three months.
- For warfarin users: INR checks twice weekly during the first month.
- Monitoring for signs of bleeding: unusual bruising, black stools, dizziness, headaches, or unexplained fatigue.
- For high-risk patients: switching to antidepressants with less platelet effect, like mirtazapine or bupropion.
But here’s the problem: 68% of inappropriate combinations happen in primary care. Many family doctors aren’t aware of the interaction-or don’t have time to dig into the data. A 2022 audit of over 12,000 records found that patients were often prescribed SSRIs and anticoagulants without any bleeding risk assessment.
What You Can Do
If you’re on an anticoagulant and your doctor suggests an SSRI:- Ask: “Is there a non-SSRI option that’s just as effective?” Mirtazapine and bupropion don’t affect platelets and are good alternatives.
- Ask: “What’s my HAS-BLED score?” If it’s 3 or higher, the risk is real.
- Ask: “Do I need more frequent blood tests?” Especially in the first month.
- Watch for signs of bleeding. Don’t wait for symptoms to get worse.
- Never stop your SSRI or anticoagulant without talking to your doctor. Stopping suddenly can cause withdrawal, stroke, or heart attack.
What’s Next?
The big unanswered question: Can we predict who’s most likely to bleed? The NIH is funding a major trial called PRECISION-AF, which is following 5,000 patients on anticoagulants who are either taking SSRIs or non-SSRI antidepressants. Results are due in late 2026. That study could finally tell us whether switching antidepressants actually reduces bleeding.The American College of Cardiology is also working on decision tools that combine depression severity scores with HAS-BLED scores to help doctors choose the safest antidepressant. That’s the future: personalized, data-driven decisions-not guesswork.
For now, the message is clear: SSRIs and anticoagulants can be used together, but not without awareness. The risk is moderate-not extreme-but it’s real. And in medicine, even moderate risks matter when they can lead to preventable hospitalizations-or worse.








Posts Comments
Erwin Kodiat January 20, 2026 AT 04:58
Been on apixaban for AFib and sertraline for anxiety for 3 years now. No issues, but I do watch for black stools like my doc told me to. Just don’t panic, stay aware. Life’s about balance, not fear.
Jake Rudin January 21, 2026 AT 14:35
So… let me get this straight: serotonin reuptake inhibition → platelet dysfunction → impaired hemostasis → increased bleeding risk? That’s not even controversial-it’s biochemistry 101. The real tragedy is that we’ve known this since 2003, and yet, primary care docs still prescribe this combo like it’s a Starbucks order. And then they wonder why ERs are full.
Astha Jain January 23, 2026 AT 07:36
omg i had no idea ssris could do this 😭 i was on citalopram and warfarin for like 2 years and never thought twice… my mom had a GI bleed last year and i thought it was just ‘old age’… now i’m kinda mad at my dr
Lydia H. January 24, 2026 AT 11:28
It’s wild how medicine still treats mental health and physical health like separate systems. You wouldn’t ignore a heart condition while treating depression-but we do this all the time. SSRIs aren’t ‘just pills’-they’re systemic modulators. We need integrated care, not silos. And honestly? The fact that this is still surprising to so many people says more about our healthcare system than about the science.
Phil Hillson January 25, 2026 AT 07:14
so like… if you’re on an SSRI and anticoagulant you’re basically just waiting to bleed out? why are we even prescribing this combo then? this is just a death sentence with a prescription label
Josh Kenna January 25, 2026 AT 19:07
Bro this is why I switched to bupropion. No platelet junk, no bleeding risk, still helps with motivation. My doc was like ‘it’s not as good for anxiety’ but honestly? I feel more like myself than I have in years. Also-stop taking ibuprofen. Just stop. Tylenol is your friend now.
Christi Steinbeck January 27, 2026 AT 13:53
YES. This is the kind of info people need to hear. I’m a nurse and I see this all the time-patients on warfarin get prescribed Zoloft and think ‘it’s just a happy pill.’ No. It’s a bleeding risk multiplier. Please, if you’re on blood thinners, ask your doc about alternatives. You deserve to feel better without risking your life.
sujit paul January 28, 2026 AT 15:17
It is written in the annals of pharmacology, yet the pharmaceutical-industrial complex continues to promote SSRIs as benign. One must ask: who profits from this silent epidemic of iatrogenic hemorrhage? The answer lies not in science, but in shareholder reports. Beware the white coat that hides the ledger.
Tracy Howard January 29, 2026 AT 03:39
Can we just talk about how Americans are so lazy they’ll take a pill for everything? In Canada, we’d go to therapy, eat better, get sunlight, and maybe try St. John’s Wort before we’d mess with serotonin like this. SSRIs are a Band-Aid on a bullet wound. And now we’re adding anticoagulants? What are we, mad scientists?
Aman Kumar January 30, 2026 AT 19:07
Platelet serotonin depletion is a well-documented phenomenon in the context of monoamine oxidase inhibition cascades. The pharmacodynamic interference with thromboxane A2 synthesis is exacerbated by concomitant COX-1 inhibition in NSAID co-administration. This is not an interaction-it’s a pharmacological collision. The data is unequivocal. The clinical negligence is unforgivable.
Valerie DeLoach February 1, 2026 AT 18:28
To everyone panicking: this doesn’t mean you can’t take SSRIs. It means you need to be informed. Talk to your doctor. Get tested. Monitor. Switch if needed. Many people live perfectly fine on this combo with proper care. The goal isn’t to scare you-it’s to empower you. Knowledge is the real medicine here.
Lewis Yeaple February 2, 2026 AT 03:41
The 33% relative risk increase cited is statistically significant (p<0.001) and clinically meaningful, with a number needed to harm of 167 patient-years. However, the absolute risk remains low for low-HAS-BLED patients. Clinical decision-making must integrate individual risk stratification-not population-level statistics alone.
Jackson Doughart February 2, 2026 AT 04:25
I’ve been on fluoxetine and rivaroxaban for five years. My INR’s stable. I get my blood work done. I don’t take NSAIDs. I eat greens. I sleep well. I’m alive. This isn’t a death sentence. It’s a reminder to be smart. If you’re careful, you can manage both. Don’t let fear silence your mental health.
Write a comment