What FeNO Testing Actually Tells You About Your Asthma
FeNO testing doesn’t just measure breath-it measures inflammation inside your airways. If you’ve ever been told your asthma isn’t well controlled, or your doctor keeps changing your inhaler without clear reasons, FeNO might be the missing piece. It’s a simple, painless test that detects nitric oxide in your exhaled breath, a chemical marker linked directly to eosinophilic inflammation-the kind that drives asthma flares and makes steroids work.
Unlike spirometry, which only shows how much air you can push out, FeNO tells you why your lungs are struggling. High levels mean your airways are inflamed, even if you feel fine. Low levels suggest your symptoms might be caused by something else-like vocal cord dysfunction or heart issues-rather than classic allergic asthma.
How the Test Works (And Why It’s So Easy)
You don’t need to be a breathing expert. The test takes less than a minute. You inhale deeply through a filter that removes outside air pollution and nitric oxide. Then, you exhale slowly and steadily into a handheld device-like blowing out a candle without puffing. The machine reads the nitric oxide level in parts per billion (ppb).
It’s that simple. No needles. No coughing. No forced breathing. Kids as young as five can do it. Adults with severe asthma who struggle with spirometry often find FeNO the first test they can actually complete reliably.
Before the test, avoid smoking, eating, drinking (except water), or exercising for at least an hour. These can throw off the reading. The device gives results in seconds. No waiting. No lab delays.
What Your FeNO Number Means
FeNO levels are interpreted differently for adults and children:
- Adults: Below 25 ppb = low inflammation; 25-50 ppb = moderate; above 50 ppb = high inflammation
- Children (5-12): Below 20 ppb = low; 20-35 ppb = moderate; above 35 ppb = high
These aren’t just numbers-they’re clinical signals. A reading above 50 ppb in an adult with wheezing and coughing strongly suggests eosinophilic asthma. That means inhaled corticosteroids will likely help. A reading below 25 ppb in someone on daily steroids might mean their medication isn’t targeting the right problem.
But here’s the catch: FeNO doesn’t work for everyone. If you’re a smoker, your levels can drop by 30-50%, even if inflammation is present. Allergic rhinitis, sinus infections, and even recent steroid use can also alter results. That’s why doctors never rely on FeNO alone.
Why FeNO Beats Blood Tests and Sputum Analysis
Doctors have other tools to check for inflammation-blood eosinophil counts, sputum tests, even allergy skin prick tests. But each has drawbacks.
Blood tests show general inflammation, not specifically in your lungs. They’re useful, but they can’t tell you if your airways are inflamed or if your lungs are reacting to something else. Sputum tests are more accurate-they look directly at cells from your lungs-but collecting sputum is messy, time-consuming, and many patients refuse it. FeNO? It’s clean, fast, and you’ll actually want to do it again next month.
Studies show FeNO correlates well with sputum eosinophils (r=0.5-0.7), meaning if your FeNO is high, chances are good your lungs are full of those inflammatory cells. Blood eosinophils? They only correlate at r=0.3-0.6. FeNO is simply a better window into your airways.

How FeNO Changes Treatment-Real Examples
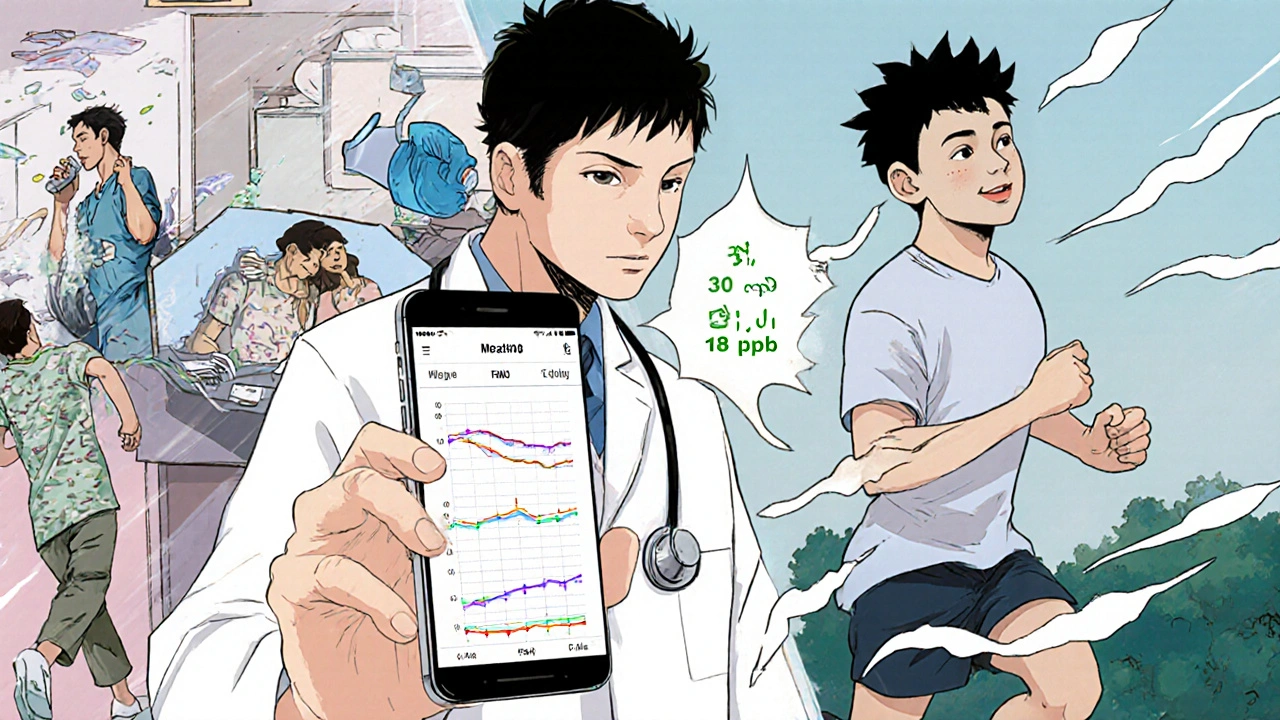
Imagine you’ve been on a high-dose inhaler for six months. You still wake up coughing. Your doctor suspects you’re not responding. A FeNO test shows 62 ppb. That’s high. So your doctor switches you to a biologic-like dupilumab-that targets the exact pathway causing the inflammation. Within weeks, your symptoms improve. Your FeNO drops to 18 ppb. You’re no longer on high-dose steroids.
That’s not hypothetical. In a 2022 study, patients whose treatment was guided by FeNO had 50% fewer asthma attacks than those managed by symptoms alone. Another study found FeNO testing helped avoid unnecessary biologics in 40% of patients who didn’t actually have type 2 inflammation.
One patient in Bristol, 34, had been misdiagnosed with chronic bronchitis for seven years. Her FeNO was 48 ppb. Her doctor realized: this wasn’t smoking-related. This was asthma. She started the right treatment. She hasn’t been to A&E in two years.
When FeNO Doesn’t Help (And Why)
FeNO isn’t magic. It only detects type 2 inflammation-the kind driven by allergies and eosinophils. If your asthma is triggered by cold air, exercise, or stress without eosinophils involved, your FeNO might be normal. That doesn’t mean your asthma isn’t real. It just means FeNO won’t pick it up.
Some people get false negatives because they didn’t follow prep instructions. Others get inconsistent results due to poor technique. That’s why trained staff use devices with real-time feedback, like the NIOX VERO®, which shows you if you’re exhaling too fast or too slow. Good technique cuts invalid results from 20% down to under 5%.
And yes, insurance can be a hurdle. In the U.S., only 58% of commercial plans cover FeNO without prior authorization. In the UK, it’s widely available through the NHS thanks to NICE guidelines. If your doctor recommends it and your insurer denies it, ask for a letter of medical necessity. Many appeals succeed when you tie the test to frequent ER visits or steroid dependence.
What’s Next for FeNO Testing
FeNO tech is getting smarter. In early 2023, the FDA cleared the first smartphone-connected FeNO device-Breathometer Asthma-that lets you track your levels at home. Your doctor can see trends over time without you having to come in every month.
Research is now looking at FeNO to predict who will respond to expensive biologics like benralizumab. If your FeNO is above 50 ppb and you’ve had three or more attacks in a year, you’re likely a strong candidate. That means fewer trials, fewer side effects, and better outcomes.
Even in rural clinics, portable FeNO devices are becoming more common. The cost of the machines has dropped, and training takes less than half an hour. The real barrier isn’t technology-it’s awareness. Many primary care doctors still don’t know how to use it.
What Patients Say About FeNO Testing
On patient forums, the feedback is clear. Of 142 people surveyed by Asthma + Lung UK, 87% called the test “very easy” or “easy.” One user wrote: “I blew into a tube for 10 seconds. Got results while my spirometry was still being set up. Finally, someone understood why I was struggling.”
On Reddit, 73% of users said FeNO helped them convince their doctor to change treatment. “I had proof my inhaler wasn’t working,” said one. “It wasn’t me being dramatic.”
But not everyone has access. Some report insurance denials. Others live in areas where no clinic offers the test. If you’re in a rural area or your doctor doesn’t offer FeNO, ask if they can refer you to an asthma specialist or respiratory clinic. It’s becoming standard care in the UK and top U.S. hospitals. You deserve the same.
How to Get the Most Out of Your FeNO Test
- Ask your doctor if FeNO is right for you-especially if you’re on daily steroids or have frequent flares.
- Follow prep rules: no smoking, eating, or exercise for one hour before.
- Don’t rush the exhale. Breathe out slowly and steadily. The device will guide you.
- Track your numbers over time. One reading tells you a story. Five readings tell you a trend.
- Combine it with spirometry and symptom logs. FeNO works best as part of a bigger picture.
FeNO testing isn’t about replacing your doctor’s judgment. It’s about giving them better data. And if you’re the one living with asthma, it’s about getting answers-fast, simple, and without a needle.
Is FeNO testing painful?
No, FeNO testing is completely painless. You simply breathe into a handheld device for about 10 seconds. There are no needles, no throat swabs, and no forced breathing. It’s often described as easier than a spirometry test and well-tolerated by children and adults alike.
How often should I get a FeNO test?
For most people on maintenance asthma therapy, FeNO testing is recommended 3-4 times per year. More frequent testing-every 1-2 months-is advised during treatment changes, after starting a new medication, or after an asthma flare. Your doctor will tailor the schedule based on your symptoms and control.
Can FeNO diagnose asthma on its own?
No. FeNO cannot diagnose asthma alone. While high levels strongly suggest eosinophilic asthma, low levels don’t rule it out. Many people with asthma have normal FeNO, especially if their asthma isn’t driven by type 2 inflammation. Diagnosis requires combining FeNO with symptoms, lung function tests, and medical history.
Why is my FeNO result different from my last test?
Small changes are normal. FeNO levels can shift due to recent smoking, illness, steroid use, or even how well you followed pre-test instructions. A big drop usually means your treatment is working. A rise might signal worsening inflammation. Trends over time matter more than single readings.
Does insurance cover FeNO testing?
Coverage varies. In the UK, NHS guidelines require access to FeNO testing. In the U.S., Medicare covers it for asthma management, but many private insurers require prior authorization. If denied, ask your doctor to submit a letter explaining how the test impacts your treatment plan. Many appeals succeed when tied to frequent exacerbations or steroid dependence.
Can I use FeNO at home?
Yes. As of early 2023, the first FDA-cleared smartphone-connected FeNO device became available for home use. These devices let you track your levels over time and share data with your doctor. While not a replacement for clinical testing, they’re useful for monitoring trends between visits, especially if you’re on biologics or adjusting your treatment.
What to Do Next
If you’ve been struggling with asthma control, ask your doctor about FeNO testing. Bring up your history: how often you use your rescue inhaler, whether you’ve had ER visits, if steroids help or don’t. If your doctor says no, ask why-and if they can refer you to a specialist. FeNO isn’t a luxury. It’s a tool that turns guesswork into evidence. And if you’re the one breathing through it every day, you deserve nothing less.







Posts Comments
Rachel Wusowicz November 16, 2025 AT 05:02
I've been tracking my FeNO for 14 months now... and I swear the device glitches every time the government runs a drone over my neighborhood. I mean, why else would my numbers drop exactly when the power grid flickers? They're not measuring nitric oxide-they're measuring my soul's resistance to surveillance. The device? It's a NSA-approved breathalyzer. I've stopped using it. I trust my coughs more than machines that whisper in ppb.
ZAK SCHADER November 17, 2025 AT 13:35
This whole FeNO thing is just another liberal healthcare scam. In America we used to treat asthma with bronchodilators and grit-not some fancy breathalyzer that costs more than my truck. And now they want kids blowing into tubes instead of learning to breathe right? Next they'll be testing your tears for patriotism levels. Wake up people.
Danish dan iwan Adventure November 19, 2025 AT 13:33
FeNO is a type-2 biomarker. Eosinophilic endotype. Not diagnostic. Not predictive. Correlational at best. Clinical utility is context-dependent. In resource-limited settings, spirometry + symptom scoring remains gold standard. Biologics are not first-line. Avoid overmedicalization.
Ankit Right-hand for this but 2 qty HK 21 November 20, 2025 AT 19:00
This is why India doesn't need this nonsense. We have 1.4 billion people breathing smog 24/7 and no one's running FeNO tests. You think a machine in a sterile clinic can measure what a lifetime of dust, diesel, and desperation does to your lungs? This is Western privilege disguised as science. Go fix your air quality before you test your breath.
Daniel Stewart November 20, 2025 AT 19:28
There's something profoundly lonely about measuring inflammation through breath. We are reduced to molecules-nitric oxide, parts per billion-as if our suffering could be quantified by a machine that doesn't care whether we slept, or cried, or held our child's hand last night. We are not data points. We are ghosts in the algorithm.
Latrisha M. November 22, 2025 AT 15:59
FeNO is a helpful tool when used correctly. It's not a replacement for clinical judgment. If you're on daily steroids and still struggling, it's worth discussing with your provider. Just make sure you follow prep guidelines-no food, smoke, or intense exercise an hour before. Consistency matters more than one reading. Track trends, not spikes.
John Mwalwala November 22, 2025 AT 23:17
Yo so I got my FeNO tested last week and it was 68 ppb-INSANE. My doc was like 'bro you're a walking cytokine storm.' So I started dupilumab and now I can run without wheezing. But here's the kicker-my roommate has the same device and his was 12 ppb and he smokes 2 packs a day. So I think the machine is calibrated for white people. Or maybe it's the wifi. I don't trust tech that doesn't ask how you're feeling.
Dan Angles November 24, 2025 AT 21:34
The clinical utility of fractional exhaled nitric oxide testing has been well-documented in peer-reviewed literature, particularly in the context of type 2-high asthma phenotypes. However, one must remain cognizant of confounding variables including but not limited to: environmental exposures, pharmacologic interventions, and technical adherence during exhalation. A multidisciplinary approach integrating pulmonary function testing, clinical history, and patient-reported outcomes remains paramount. The device is an adjunct-not an arbiter.
Write a comment