Medication Dose Adjuster Calculator
This tool helps you understand how your individual factors affect medication dosing for drugs with narrow therapeutic index (NTI). Enter your details to see recommended dose ranges.
Recommended Dose Range
Safe Range
This is the therapeutic window where the medication works without serious side effects.
Danger Zone
Doses outside this range may cause toxicity or loss of effectiveness.
Why this matters: For NTI drugs like warfarin and digoxin, the difference between a therapeutic dose and a toxic dose is very small. Your individual factors directly impact this balance.
Getting the right dose of medication isn’t just about following the label. It’s about finding the sweet spot where the drug works - without hurting you. Too little, and it does nothing. Too much, and you could end up in the hospital. For many people, especially those on long-term meds, this balancing act is constant, confusing, and sometimes dangerous.
Why One Size Doesn’t Fit All
Doctors don’t just pick a dose out of thin air. But for decades, the standard approach was simple: start with the average adult dose. That’s what the clinical trials used. But what if you’re 80? Or weigh 45kg? Or have kidneys that don’t filter like they used to? That average dose might be too high - or too low. Take digoxin, a heart medication. Just two and a half times the normal dose can kill half the people who take it. That’s not a typo. It’s a narrow therapeutic index - meaning the gap between a helpful dose and a deadly one is razor-thin. Warfarin, phenytoin, and lithium are the same. For these drugs, even small mistakes in dosing can lead to strokes, seizures, or heart failure. Meanwhile, for drugs like penicillin, the window is wide. You can take more or less without much risk. But for NTI (narrow therapeutic index) drugs, every milligram counts. And that’s where personalization becomes non-negotiable.What Makes Your Dose Unique
Your body doesn’t process medicine the same way as your neighbor’s. Five key factors change how a drug behaves in you:- Age: After 65, your liver and kidneys slow down. Many seniors need 20-30% less of certain drugs just to stay safe.
- Weight: Obesity changes how drugs spread in your body. For some meds, dosing is based on ideal body weight - not your actual weight. Add 40% of your extra weight to your ideal, and that’s often the starting point.
- Kidney function: Creatinine clearance is the gold standard. If it’s below 60 mL/min, many drugs need lower doses. Many GPs don’t check this regularly - but they should.
- Liver health: The Child-Pugh score tells you how well your liver metabolizes drugs. If you have cirrhosis, even common painkillers can build up to toxic levels.
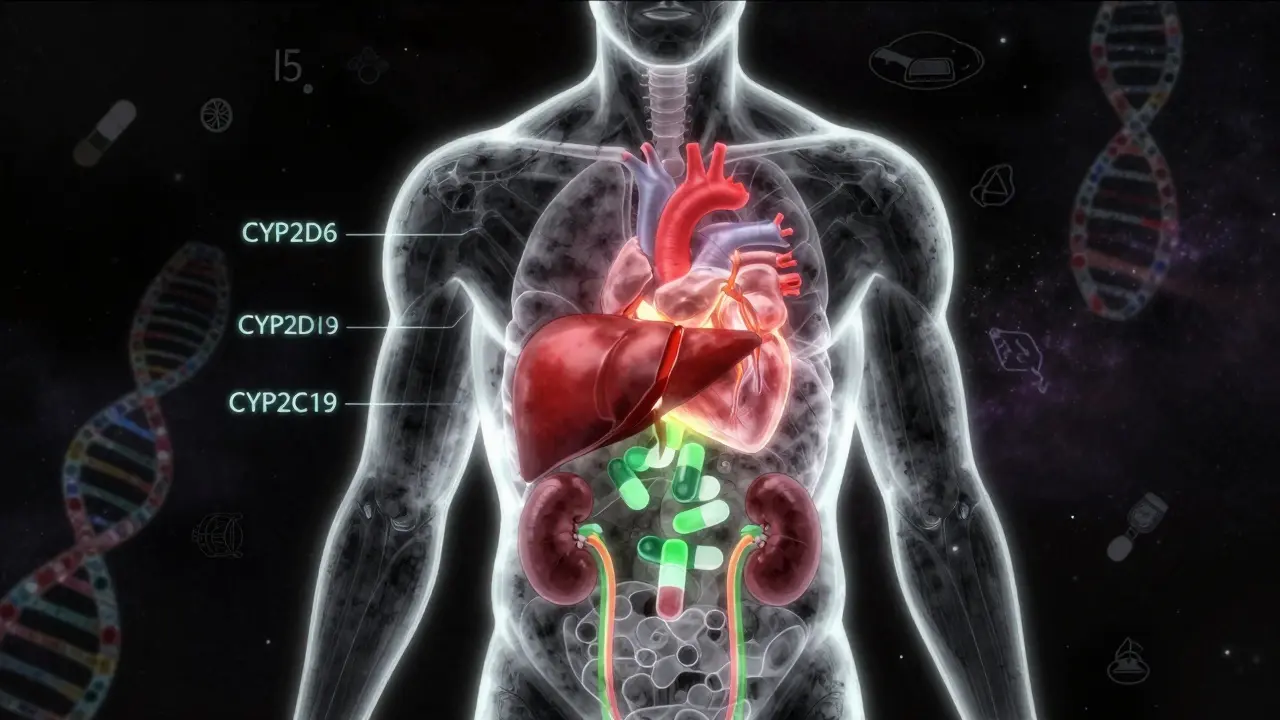
- Genes: About 25% of commonly prescribed drugs are affected by genetic variations. If you’re a slow metabolizer of CYP2D6 or CYP2C19, you could overdose on standard doses of antidepressants, beta-blockers, or blood thinners.
NTI Drugs: When Monitoring Isn’t Optional
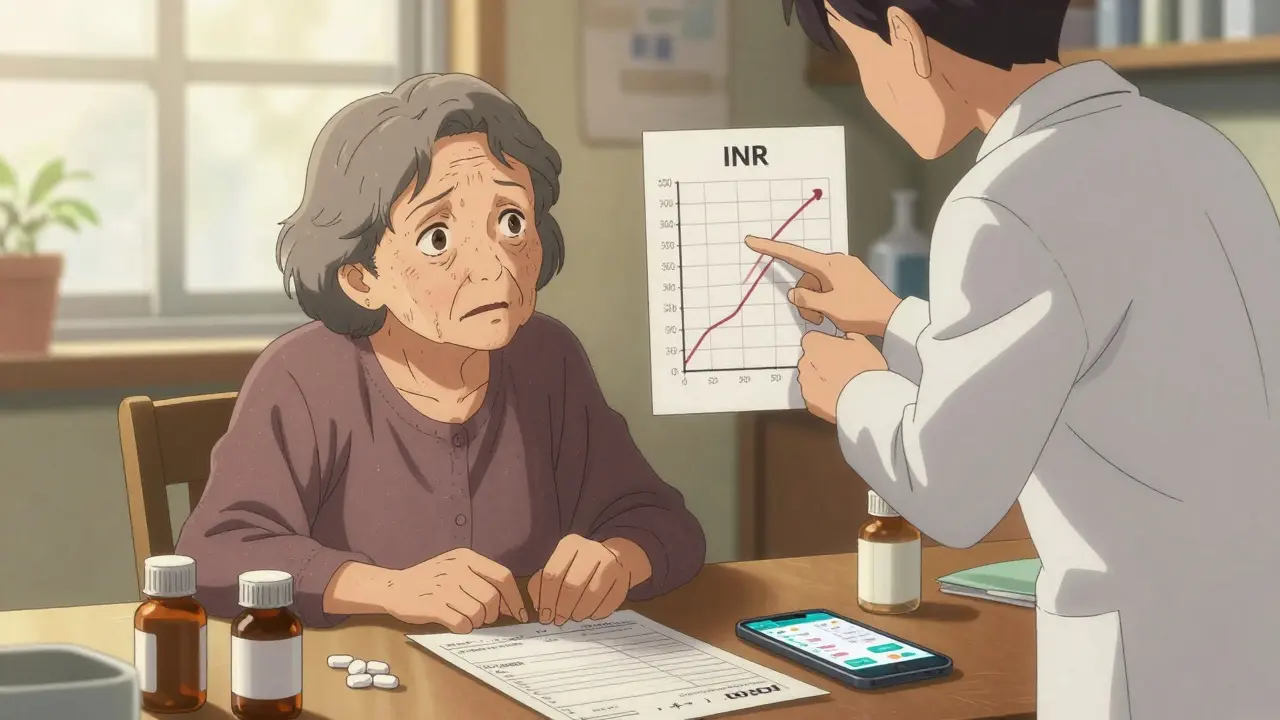
For drugs with a therapeutic index of 2 or 3, regular blood tests aren’t a luxury - they’re life insurance.- Warfarin: Requires INR checks every 2-4 weeks. Target range: 2.0-3.0. Go above 4.0, and you risk internal bleeding. Below 1.8, and clots form.
- Digoxin: Blood levels above 2.0 ng/mL are toxic. Even small changes in potassium (from diuretics or diet) can push levels into danger.
- Phenytoin: Used for seizures. Too low? Seizures return. Too high? Tremors, confusion, even coma.
The Real Cost of Guesswork
Most clinical trials exclude older adults, pregnant women, and people on five or more drugs. Yet these are the people who need dose adjustments the most. That’s a gap. A dangerous one. In the UK, 44% of adults over 65 take five or more medications. That’s called polypharmacy. And it triples your risk of a bad reaction. One study showed that pharmacist-led reviews reduced hospital admissions by 22% in this group. Why? Because pharmacists don’t just count pills. They look at interactions, kidney function, timing, and even whether the patient can open the bottle. Meanwhile, drug companies often set prices based on what the market will bear - not what’s clinically necessary. High-dose statins might lower cholesterol a little more, but the benefit is tiny. The risk of muscle damage, liver stress, or diabetes? Not so small. Yet guidelines still push for maximum doses. That’s not medicine. That’s volume.What Works: Precision, Not Protocol
The future isn’t about rigid rules. It’s about data. - Pharmacist-led clinics for anticoagulants have cut major bleeding by 60% in warfarin users. - Clinical decision tools now use real-world data - age, weight, genetics, labs - to suggest doses in seconds. Companies like DoseMe and InsightRX are building AI models that outperform traditional formulas by 25-40%. - Therapeutic drug monitoring is growing fast. The global market will hit $3.5 billion by 2029. That’s because doctors are finally realizing: you can’t manage what you don’t measure. Even in primary care, simple steps help:- Ask: “What’s your creatinine clearance?”
- Review all meds - including supplements - every 6 months.
- Deprescribe: If a drug isn’t clearly helping, stop it. Less is often more.
- Use apps or pill organizers with alerts - but don’t rely on them alone.
What to Do If You’re on a High-Risk Drug
If you’re taking warfarin, digoxin, lithium, or phenytoin, here’s your action plan:- Know your target level. Ask your doctor or pharmacist for the exact range.
- Get blood tests on schedule. Don’t skip them because you “feel fine.”
- Keep a log. Note any new symptoms: dizziness, nausea, unusual bruising, confusion.
- Tell every new provider - even your dentist - what you’re taking. Many interactions happen when you’re not thinking about meds.
- Ask: “Is this dose right for me?” Don’t assume it is.
The Bottom Line
Medication isn’t a one-time fix. It’s a dynamic tool. What works today might be too much tomorrow. Your body changes. Your health changes. Your other meds change. The goal isn’t to take the most or the least. It’s to take the right amount. For you. Right now. That means asking questions. Tracking symptoms. Demanding lab work when needed. And trusting your pharmacist - they’re trained for this. They see the interactions, the gaps, the risks your doctor might miss in a 10-minute appointment. This isn’t about being difficult. It’s about being informed. Because when it comes to your meds, you’re not just a patient. You’re the most important part of the equation.What is a narrow therapeutic index (NTI) drug?
A narrow therapeutic index (NTI) drug has a very small difference between the dose that works and the dose that causes harm. The therapeutic index is 2-3 or lower. Examples include warfarin, digoxin, phenytoin, and lithium. Even small changes in dose or how your body processes the drug can lead to serious side effects or toxicity. These drugs almost always require regular blood tests to monitor levels.
Can I adjust my own medication dose if I feel it’s too strong or too weak?
Never adjust your dose without talking to your doctor or pharmacist. Even if you think you know what’s happening - like feeling more tired or less effective - changing the dose yourself can be dangerous. With NTI drugs, a small change can lead to overdose or loss of effectiveness. Always report symptoms, then let your provider decide whether to adjust the dose based on tests and your full medical picture.
Why do some medications need blood tests while others don’t?
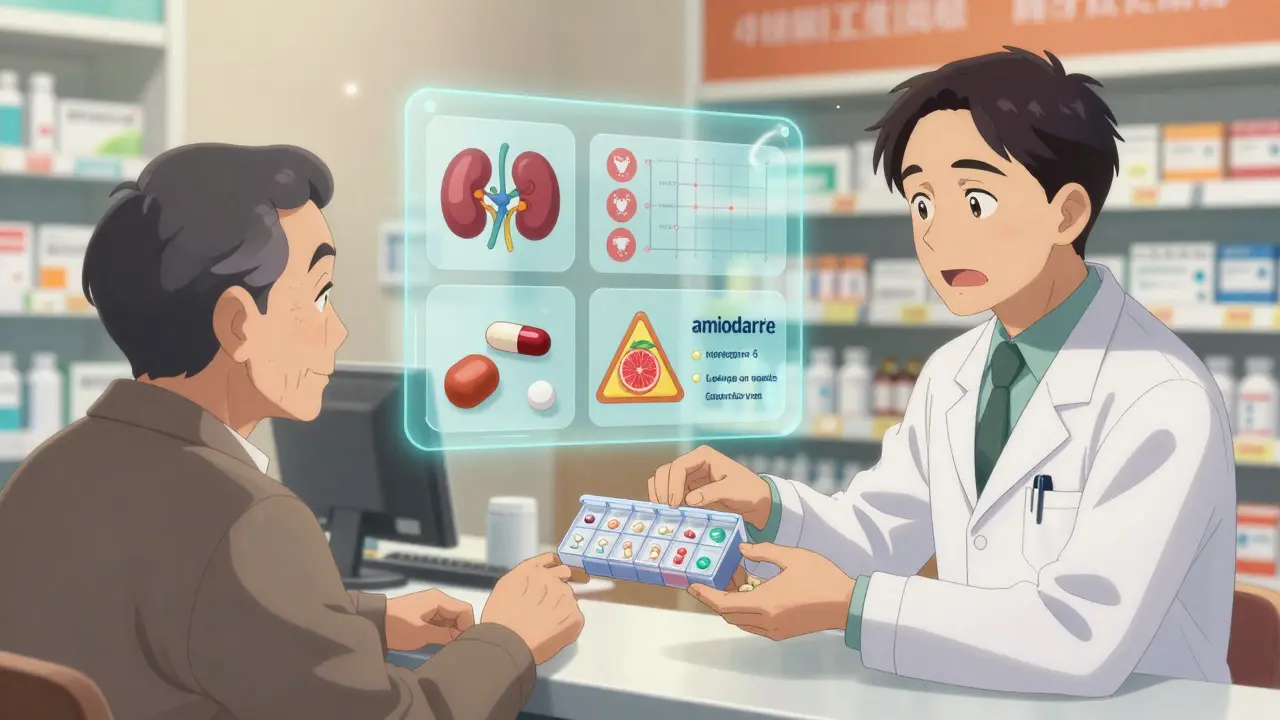
Blood tests are needed when the difference between a helpful dose and a harmful one is very small - that’s the narrow therapeutic index. Drugs like warfarin or digoxin have no safety margin. If levels are too high, you bleed or get poisoned. If too low, you get a clot or seizure. For drugs like amoxicillin or ibuprofen, the safety window is wide, so routine blood tests aren’t needed. But for NTI drugs, monitoring isn’t optional - it’s essential.
How do age and kidney function affect medication dosing?
As you age, your kidneys and liver work slower, so drugs stay in your body longer. This can cause buildup and toxicity. Kidney function is measured by creatinine clearance. If it’s below 60 mL/min, many drugs need lower doses - sometimes 30-50% less. Many older adults are on meds that were never tested in people with reduced kidney function, so their doses may be too high. Always ask for your creatinine clearance result - don’t assume it’s fine just because your blood test looked normal.
What should I do if I’m taking five or more medications?
If you’re on five or more meds, you’re at high risk for interactions and side effects. Request a full medication review with your GP or pharmacist. Bring every pill bottle - including vitamins and supplements. Ask: “Which of these are still necessary?” “Are any of these interacting?” “Could any dose be lowered?” Studies show this reduces hospital visits by 22%. Don’t wait until something goes wrong. Proactive reviews save lives.







Posts Comments
Abby Polhill December 25, 2025 AT 02:06
NTI drugs are the silent killers in polypharmacy. I work in a geriatric clinic and see this daily - someone on warfarin, amiodarone, and a diuretic with a creatinine clearance of 42 and no one checking INR for three months. It’s not negligence, it’s systemic. The system is built for volume, not precision. And the worst part? The patient thinks they’re fine because they ‘don’t feel different.’
Pharmacists are the unsung heroes here. We need more of them embedded in primary care, not just dispensing scripts. DoseMe and InsightRX? Game changers. AI isn’t replacing doctors - it’s giving them the data they should’ve had decades ago.
Delilah Rose December 26, 2025 AT 19:02
I’ve been on lithium for bipolar for 17 years, and I can tell you - it’s not about the pill, it’s about the rhythm. The blood tests, the kidney checks, the sodium intake, the hydration, the weather changes affecting how my body holds onto it - it’s a full-time job. My doctor used to just say ‘take it daily’ and call it a day. Then I found a clinical pharmacist who actually looked at my trends over time, not just the one lab result. That’s when my mood stabilized for the first time in a decade.
It’s not magic. It’s monitoring. It’s listening. It’s not assuming that because you’re 60, you’re automatically on the ‘old person dose.’ My body doesn’t care about age charts - it cares about what’s in it, and how fast it leaves. And if your provider won’t talk about that, find someone who will. Your life depends on it.
Spencer Garcia December 27, 2025 AT 12:38
Agreed. Creatinine clearance is the first thing you should ask for. Not serum creatinine. Clearance. Most GPs don’t know the difference. If you’re over 65 or on multiple meds, insist on it. It’s free with a basic CMP. Small step, huge impact.
Jillian Angus December 28, 2025 AT 05:43
my dr never checked my creatinine for years even though i was on lisinopril and metformin
then i had a bad reaction and they finally did
turns out i was at 48
they lowered everything and i stopped feeling like a zombie
Ajay Sangani December 28, 2025 AT 23:33
you know what is truely sad? we have the tech to personalize dosing down to the gene level but we still rely on weight charts from the 1980s and doctor intuition. it is not just about medicine, it is about how we value human biology. we treat bodies like machines with one setting, but they are more like ecosystems. a change in one part affects all others. and yet we keep prescribing like we are filling a coffee mug, not tuning a symphony.
Pankaj Chaudhary IPS December 29, 2025 AT 10:19
As a medical professional in India, I can confirm that the lack of therapeutic drug monitoring is a systemic crisis. In rural clinics, patients are given standard doses of phenytoin or digoxin without any lab support. Many end up with toxicity or uncontrolled seizures. The solution lies not in more doctors, but in training community pharmacists to perform basic monitoring and refer appropriately. Mobile health units with point-of-care testing could revolutionize care in low-resource settings. This is not a Western problem - it is a global human rights issue.
Katie Taylor December 30, 2025 AT 04:22
STOP letting doctors gaslight you. ‘You feel fine?’ That’s not a reason to skip your INR. That’s the exact moment you need it most. I had a stroke because my warfarin was too low and my doctor said ‘you look good.’ Look good? I was a walking clot. Now I do my own INR at home with a machine. It’s $50 a strip. Worth every penny. If your doctor won’t support you - fire them. Your life is not a suggestion.
Isaac Bonillo Alcaina December 31, 2025 AT 10:32
Let’s be honest: most of this is just glorified common sense. If you’re old, overweight, or on five meds - you’re a walking liability. The real issue isn’t dosing algorithms - it’s that people refuse to take responsibility. Stop blaming the system. Stop expecting your doctor to be your pharmacist, your nutritionist, and your therapist. If you can’t manage your meds, don’t take them. Or better yet - don’t get sick in the first place. Prevention isn’t a buzzword. It’s a lifestyle. And most people aren’t willing to do the work.
Bhargav Patel January 1, 2026 AT 09:16
There is a profound philosophical tension here: medicine seeks to universalize through protocols, yet biology is inherently individual. We quantify, we standardize, we reduce - but the human body resists reduction. The narrow therapeutic index is not merely a pharmacological fact; it is a metaphor for the limits of our control. We can measure, model, and predict - but we cannot fully command. Perhaps the true art of medicine lies not in perfecting the dose, but in humbly acknowledging the mystery of the body’s response - and listening, deeply, to the patient who lives within it.
Steven Mayer January 2, 2026 AT 12:55
AI dose models are just statistical noise wrapped in a white coat. They’re trained on biased datasets - mostly white, male, young adults. What happens when you plug in a 78-year-old South Asian woman with CKD and a CYP2C19 poor metabolizer variant? The algorithm spits out a number. The doctor trusts it. The patient bleeds out. We’re outsourcing judgment to code written by people who’ve never held a patient’s hand during a seizure. This isn’t progress. It’s automation of arrogance.
Bartholomew Henry Allen January 4, 2026 AT 04:12
Why are we letting foreigners design our drug guidelines? American patients need American dosing. Our bodies are different. Our genetics are different. Our healthcare system is different. Why are we following European studies? Why are we using BMI from Asia? We need U.S.-only clinical trials. No more global one-size-fits-all. We need American precision. American safety. American medicine.
Jeffrey Frye January 4, 2026 AT 07:08
so i was on lithium for like 5 years and my doc never checked levels until i started shaking and couldn’t walk
turns out i was at 1.8 and the upper limit is 1.2
he said ‘oh i thought you were fine’
yeah i was fine until i couldn’t hold a fork
now i have to take it every other day and i’m still scared to sleep
Raja P January 5, 2026 AT 10:49
i just want to say thank you to the pharmacist who sat with me for an hour last week and asked me if i could open my pill bottles
no one had ever asked that before
i have arthritis and was just crushing them in my palm
now i have a easy-open dispenser and i haven’t missed a dose since
Joseph Manuel January 6, 2026 AT 07:33
The assertion that pharmacists reduce hospital admissions by 22% is statistically insignificant in the context of national healthcare expenditure. The cost of pharmacist-led interventions far outweighs the marginal benefit. Furthermore, the reliance on genetic testing and AI-driven dosing represents an unnecessary commodification of patient care. Standardized protocols, though imperfect, ensure consistency and reduce liability. The current trend toward hyper-personalization is not evidence-based - it is market-driven.
Write a comment