Corticosteroid Psychosis Risk Calculator
Dose Input
Enter your corticosteroid dose in milligrams per day (mg/day) of Prednisone equivalent.
Risk Assessment Results
Estimated Risk:
Based on clinical data: Below 40 mg/day: ~1.3% risk; 40-80 mg/day: ~10% risk; Above 80 mg/day: up to 18.4% risk
When doctors prescribe Corticosteroids are a class of anti‑inflammatory and immunosuppressant drugs that have saved countless lives. They work by mimicking the body’s natural cortisol hormone to calm down overactive immune responses, but the trade‑off can be a bewildering range of mood and behavioral shifts - from mild irritability to full‑blown psychosis.
Why Mood Changes Matter
Patients often notice the first hints of trouble within days of starting therapy: trouble sleeping, sudden euphoria, or a rapid swing from upbeat to down. If these red flags are missed, the condition can spiral into severe depression, mania, or corticosteroid psychosis. This isn’t a rare curiosity; studies show that 5 % to 18 % of people on high‑dose regimens develop serious psychiatric symptoms.
How Often Does It Happen?
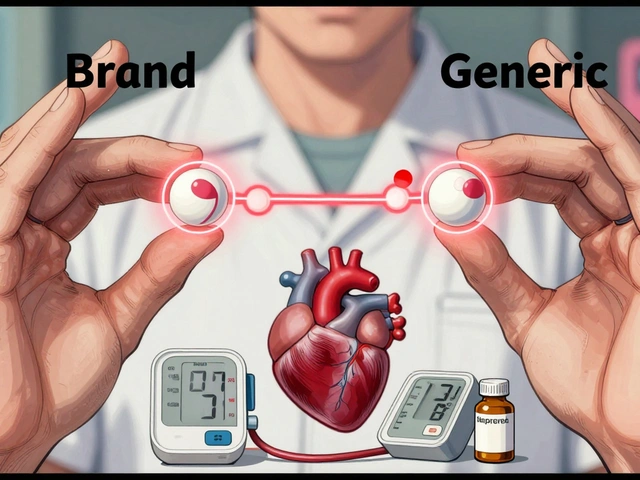
Data collected over the last two decades paint a clear dose‑response picture:
- Below 40 mg/day of Prednisone - about 1.3 % risk.
- 40 mg-80 mg/day - risk climbs to roughly 10 %.
- Above 80 mg/day - up to 18.4 % of patients see psychiatric effects.
Older adults (65 +), women, and anyone with a prior mood disorder is especially vulnerable.
What Symptoms Look Like
The symptom spectrum spans several categories:
- Euphoria - reported in about 27 % of cases; patients feel unusually upbeat or hyper‑confident.
- Insomnia - the most common early sign, affecting roughly 42 %.
- Mood swings - rapid shifts between irritability, sadness, and elation.
- Personality changes - patients may become unusually aggressive or withdrawn.
- Severe depression - seen in 14-15 % of users, sometimes with suicidal thoughts.
- Psychosis - delusions, hallucinations, or disorganized thinking; occurs in 5-18 % of high‑dose users.
Memory problems, especially with verbal and declarative recall, often accompany the above, hinting at hippocampal involvement.
What’s Going on Inside the Brain?
Researchers still debate the exact mechanisms, but three pathways dominate the conversation:
- Suppression of the HPA axis - Corticosteroids blunt the body’s stress‑response loop, indirectly altering neurotransmitter balance.
- Hippocampal toxicity - High cortisol levels can shrink hippocampal neurons, compromising memory and mood regulation.
- Dopamine surge - Animal studies show steroids boost tyrosine hydroxylase, raising dopamine and potentially triggering psychotic features.
These pathways often overlap, making each patient’s presentation unique.

How to Spot It Early
Time is crucial. Most psychiatric signs appear within the first 3‑5 days of therapy, but they can emerge later or even after a taper. Key early alerts include:
- Sudden anxiety or restlessness.
- Unexplained confusion or disorientation.
- Rapid mood elevation or depressive episodes.
- Insomnia that worsens despite sleep hygiene.
When any of these surface, clinicians should pause to evaluate, ideally using a standardized rating tool - a recommendation echoed across recent guidelines.
Diagnosing Corticosteroid‑Induced Psychosis
According to the DSM‑5, the diagnosis hinges on three criteria:
- Prominent psychotic symptoms (delusions, hallucinations, disorganized speech/behavior).
- Onset during or shortly after steroid exposure.
- Exclusion of other causes - substance use, metabolic disturbances, primary psychiatric illnesses.
Because steroids can mask or mimic other conditions, a thorough work‑up (blood tests, imaging if needed) is essential before labeling the event as steroid‑related.
Management Strategies
Once identified, the best first step is to lower the steroid burden:
- Reduce Prednisone to < 40 mg/day (or dexamethasone to ≤6 mg oral). In many cases, symptoms fade within a week of tapering.
- If tapering isn’t possible (e.g., for life‑threatening inflammation), add a psychotropic medication.
Medication choices are off‑label but supported by case series:
| Drug | Typical Dose | Onset of Relief |
|---|---|---|
| Haloperidol | 0.5-1 mg/day | Days |
| Olanzapine | 2.5-20 mg/day | 1-2 weeks |
| Risperidone | 1-4 mg/day | Days to a week |
Lithium can prevent manic spikes but requires close monitoring for renal and thyroid side effects, so it’s usually reserved for patients with a known bipolar history.
Collaboration is key: primary care, the prescribing specialist (pulmonology, rheumatology, nephrology), and a liaison psychiatrist should discuss the taper plan and any adjunct meds.
Patient Education Checklist
Empowering patients cuts down on surprises:
- Explain the possibility of mood changes before starting therapy.
- Provide a one‑page handout listing early warning signs.
- Set a follow‑up call within 48-72 hours of the first dose for high‑risk regimens.
- Encourage family members to monitor behavior and report concerning shifts.
Future Directions & Research Gaps
Despite decades of awareness, we still lack:
- Standardized, validated assessment tools for steroid‑induced psychiatric effects.
- Biomarkers to predict who will develop severe symptoms.
- FDA‑approved treatments specifically targeting this condition.
Recent calls from Frontiers in Pharmacology urge the development of "clinimetric methods" - quantitative scales that could be baked into electronic health records for real‑time alerts.
Key Takeaways
- High‑dose corticosteroids can trigger a spectrum of psychiatric symptoms, with psychosis affecting up to 1 in 6 high‑risk patients.
- Risk climbs sharply above 40 mg/day of Prednisone and in women, older adults, or those with prior mood disorders.
- Early detection (within the first week) and prompt tapering are the most effective interventions.
- When tapering isn’t possible, low‑dose antipsychotics such as haloperidol, olanzapine, or risperidone are the go‑to options.
- Patient education and multidisciplinary coordination dramatically reduce the chance of severe outcomes.
How quickly can mood changes appear after starting steroids?
Most patients notice anxiety, insomnia, or irritability within the first 3‑5 days. Severe symptoms like psychosis can emerge anytime during the first few weeks.
Is there a safe lower limit for prednisone that eliminates psychiatric risk?
Risk drops dramatically below 40 mg/day, but even low doses can affect vulnerable individuals. Monitoring is still advised for anyone with a psychiatric history.
Can steroid‑induced psychosis persist after the drug is stopped?
Yes. Case reports from 2025 show that psychotic and manic symptoms sometimes linger for weeks after tapering, indicating a need for follow‑up care.
What are the first‑line antipsychotics for steroid‑induced psychosis?
Low‑dose haloperidol (0.5-1 mg/day), olanzapine (2.5-20 mg/day), or risperidone (1-4 mg/day) have the most documented success.
Should family members be involved in monitoring?
Absolutely. Loved ones often notice subtle personality shifts sooner than clinicians, so encouraging them to report changes can speed intervention.






Posts Comments
Olivia Harrison October 25, 2025 AT 13:15
Thanks for pulling together all this info! It really helps patients and clinicians see the whole picture without getting lost in jargon. The dose‑response curve you highlighted makes it crystal clear why we try to keep prednisone below 40 mg whenever possible. I also love the practical checklist – giving families a one‑page handout can make a huge difference. If anyone’s starting a high‑dose regimen, a quick call within the first 48 hours is a solid safety net.
Stay safe out there!
Bianca Larasati November 7, 2025 AT 05:49
Wow, this article hits the nail on the head!! The roller‑coaster of emotions you described is exactly what I saw in my aunt’s chart – from euphoric highs to sleepless nights in days. It’s scary how quickly those mood swings can turn into full‑blown psychosis.
We need to shout this from the rooftops so nobody gets caught off guard!
Corrine Johnson November 19, 2025 AT 23:22
One must contemplate, dear readers, the paradoxical nature of steroids – they soothe the body yet torpedo the mind, a duality that is as ancient as the humankind's quest for control;
the literature, replete with percentages, masks the individual stories that bleed behind each statistic, urging us to look beyond the numbers;
in this swirling vortex of neurochemistry, the HPA‑axis suppression stands as both culprit and sentinel, a Janus‑faced deity of homeostasis;
let us not forget that hippocampal toxicity, while subtle, erodes the very foundations of memory, leaving patients adrift in a fog of forgetting;
therefore, a vigilant eye, a compassionate ear, and a judicious taper are our only armor against this silent storm.
Buddy Bryan December 2, 2025 AT 16:55
Listen up – if you’re on a high dose and you can’t drop it, you better have an antipsychotic on standby. Haloperidol isn’t fancy, but it works fast, and you don’t have time for trial‑and‑error when someone’s sanity is on the line. Don’t wait for a crisis to call a psychiatrist; involve them early and keep the dosage as low as you can. The data is clear: above 80 mg the risk rockets, so act now.
Brett Witcher December 15, 2025 AT 10:29
The phenomenon of corticosteroid‑induced psychiatric disturbance warrants a nuanced appraisal that transcends the simplistic dose‑centric dogma historically propagated within clinical curricula.
First, it is imperative to recognize that the neuroendocrine perturbations precipitated by exogenous glucocorticoids orchestrate a cascade of molecular events, notably the dysregulation of the hypothalamic‑pituitary‑adrenal axis, which in turn modulates dopaminergic tone within mesolimbic circuits.
Second, empirical observations delineate a non‑linear relationship between cumulative prednisone exposure and the incidence of affective lability, thereby challenging the conventional threshold of 40 mg as a binary demarcation.
Third, demographic variables such as advanced age, female sex, and pre‑existing mood disorders constitute salient risk modifiers that must be integrated into individualized risk stratification algorithms.
Fourth, the latency period of symptom emergence, typically confined to the initial 3‑5 days post‑initiation, underscores the necessity for proactive monitoring protocols, including validated psychometric instruments administered at baseline and serially thereafter.
Fifth, the therapeutic armamentarium, while presently reliant on off‑label antipsychotics such as haloperidol, olanzapine, and risperidone, suffers from a paucity of randomized controlled trials, rendering evidence‑based dosing regimens provisional at best.
Sixth, the role of lithium as a prophylactic agent, though mechanistically plausible via stabilization of intracellular signaling pathways, remains circumscribed by its narrow therapeutic index and requisite renal monitoring.
Seventh, interdisciplinary collaboration – encompassing primary care, the prescribing subspecialist, and psychiatric services – is not merely advisable but essential to mitigate morbidity.
Eighth, patient education materials, when crafted with clarity and cultural competence, have demonstrable efficacy in fostering early self‑recognition of neuropsychiatric red flags.
Ninth, the current lacuna in standardized assessment tools impedes systematic data collection, thereby attenuating our capacity to conduct meta‑analyses and to refine predictive models.
Tenth, emerging research into corticosteroid‑induced hippocampal atrophy via high‑resolution neuroimaging holds promise for elucidating pathophysiological substrates, yet remains nascent.
Eleventh, the prospect of pharmacogenomic profiling to identify susceptibility loci represents a frontier that could revolutionize preemptive strategies.
Twelfth, regulatory bodies have yet to endorse any FDA‑approved pharmacotherapy expressly for steroid‑induced psychosis, a conspicuous gap in therapeutic guidance.
Thirteenth, longitudinal follow‑up studies indicate that neuropsychiatric sequelae may persist beyond taper completion, necessitating vigilance even after drug cessation.
Fourteenth, the ethical imperative to obtain informed consent that transparently communicates these risks cannot be overstated, lest we compromise patient autonomy.
Fifteenth, future directions must prioritize the development of validated, electronic health record‑integrated alert systems to flag high‑risk prescriptions in real time.
In summation, while corticosteroids remain indispensable in modern medicine, their neuropsychiatric side‑effect profile demands a sophisticated, multimodal approach that integrates risk assessment, early detection, judicious dosing, and coordinated care.
Jonah O December 28, 2025 AT 04:02
Dont trust the pharma they hide the mind control side effects!!
Aaron Kuan January 9, 2026 AT 21:35
Glucose spikes, mood dips – steroids pull the strings.
Benjamin Sequeira benavente January 22, 2026 AT 15:09
Alright, let’s get real – steroids can feel like a double‑edged sword, but you don’t have to be a martyr to survive them. The first thing I do with anyone on a high‑dose course is set a clear alarm on my phone for day three; that’s when insomnia and anxiety usually start knocking. If the patient mentions “I’m on a roller coaster,” it’s my cue to pull the trigger on a low‑dose antipsychotic, preferably something with a quick onset like haloperidol. I also make sure the prescribing specialist knows we’re not just talking about inflammation, we’re talking about the brain, too. In my clinic, I give families a one‑pager that lists “Early Warning Signs” – sudden irritability, sleeplessness, any bizarre thoughts – and I ask them to call me within 24 hours if anything pops up. Lastly, I never underestimate tapering; dropping the dose by even 10 % every few days can make the difference between a smooth ride and a psychotic plunge.
Write a comment