Many people say they’re "allergic" to a drug because it gave them a stomachache, a rash, or made them feel dizzy. But here’s the truth: most of those aren’t allergies at all. They’re side effects. And confusing the two can cost you more than just discomfort-it can limit your treatment options, raise your medical bills, and even put your health at risk.
What Exactly Is a Side Effect?
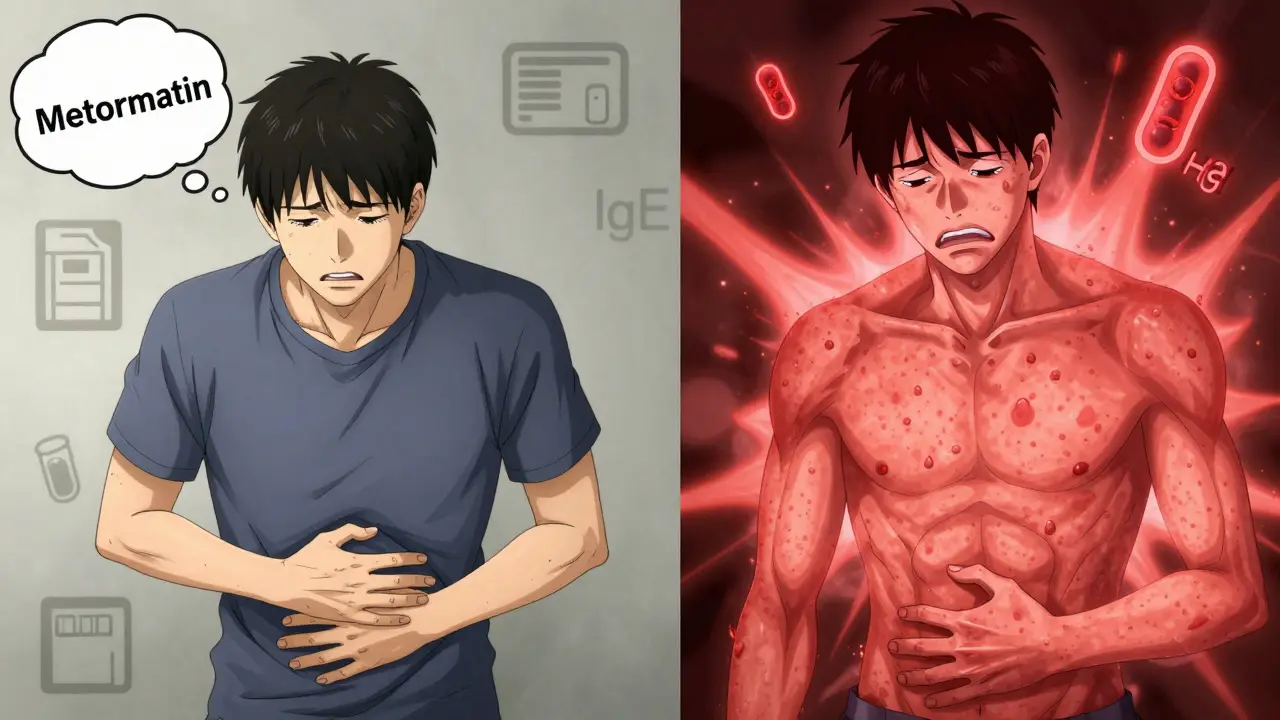
A side effect is a known, predictable reaction to a drug that happens because of how the drug works in your body. It’s not your immune system going haywire. It’s just the drug doing something it wasn’t meant to do-like causing nausea when it’s supposed to lower blood pressure. For example, metformin, a common diabetes medication, causes stomach upset in 20-30% of users. Statins, used to lower cholesterol, can cause muscle aches in 5-10% of people. These aren’t surprises. They’re listed right on the drug’s label with exact percentages. And guess what? Most of them fade over time. About 70-80% of common side effects go away after a few weeks as your body adjusts. Side effects are usually dose-related. Take more of the drug? The side effect gets worse. Take less? It often gets better. That’s why doctors might tell you to take a pill with food, or switch to a lower dose. No need to avoid the drug entirely-just tweak how you use it.What Makes a Drug Allergy Different?
A true drug allergy is your immune system mistaking the medication for a dangerous invader-like a virus or bacteria-and launching an attack. This isn’t about how the drug works. It’s about your body’s defense system going rogue. The most common allergic reactions involve Immunoglobulin E (IgE) antibodies. These kick in fast-within minutes to two hours. Symptoms? Hives, swelling of the lips or tongue, trouble breathing, a sudden drop in blood pressure. That’s anaphylaxis. It’s rare-happening in only 0.05-0.5% of drug exposures-but it’s life-threatening. Death rates are low (0.3-1%), but only if treated right away. Then there are delayed reactions. These show up days later. Think of a red, itchy rash that spreads over your chest and back. This is often T-cell mediated and common with antibiotics like penicillin or sulfa drugs. Unlike side effects, these don’t get better with lower doses. They get worse with every exposure.Penicillin: The Most Misunderstood Allergy
Penicillin is the poster child for this confusion. About 10% of Americans say they’re allergic to it. But when tested properly, 80-90% of them aren’t. That’s not a typo. Eight out of ten people who think they’re allergic to penicillin can safely take it again. Why does this matter? Because if you’re labeled "penicillin allergic," doctors avoid the best, cheapest, most targeted antibiotics. Instead, they give you broader-spectrum drugs like vancomycin or clindamycin. These are more expensive, less effective against common infections, and increase your risk of dangerous superbugs like MRSA. Studies show that mislabeled penicillin allergies lead to a 69% higher chance of MRSA infection. And the cost? It adds about $4,000 per patient per year in extra healthcare spending. That’s not just money-it’s longer hospital stays, more side effects from stronger drugs, and higher chances of treatment failure.
How Do Doctors Tell the Difference?
It’s not guesswork. There’s a clear process. First, they ask detailed questions: When did the reaction happen? How long after taking the drug? What exactly happened? Did you have hives? Swelling? Trouble breathing? Or just nausea and diarrhea? Timing is everything. An allergic reaction happens fast-or it’s delayed, but never vague. For suspected penicillin allergy, the standard is a three-step check:- History review-If your reaction was mild (like a rash without swelling or breathing issues), you might be low risk.
- Skin test-A tiny amount of penicillin is placed under your skin. If you’re truly allergic, you’ll get a red, itchy bump within 15-20 minutes. This test is 97% accurate at ruling out allergy.
- Oral challenge-If the skin test is negative, you’re given a small dose of penicillin under supervision. Less than 0.2% of low-risk patients react. If nothing happens? You’re cleared.
Why So Many People Get It Wrong
People mix up side effects and allergies because the symptoms sometimes look similar. A rash? That’s an allergy-or is it just a side effect? Diarrhea? That’s a side effect. But if you’ve had it before, you might say, "I’m allergic to this pill." A 2023 survey of over 5,000 patients found that 65% couldn’t tell the difference. The biggest mix-ups? Antibiotics and statins. People say they’re allergic to amoxicillin because it gave them diarrhea. Or they think they’re allergic to atorvastatin because they got muscle pain. Neither is an allergy. Both are side effects. Even doctors sometimes get it wrong. In one study, 90-95% of patients labeled "allergic" in their medical records didn’t have a true allergy when tested by an allergist. That’s because many reactions were never properly evaluated. And once a label sticks, it’s hard to remove-even if the patient can’t remember the details of the original reaction.What Happens When You’re Misdiagnosed
The consequences aren’t theoretical. They’re real-and costly. - A person with a false penicillin allergy might get clindamycin for a sinus infection. Clindamycin can cause C. diff, a severe, life-threatening gut infection. The risk goes up by 30-50% compared to penicillin. - Hospital stays get longer. On average, patients with a mislabeled allergy stay half a day to a day and a half longer than those who can take the right drug. - Healthcare costs in the U.S. jump by $1.1 billion a year just because people think they’re allergic to drugs they’re not. And then there’s the emotional toll. Someone might avoid life-saving antibiotics because they think they’re allergic. Or they might skip a needed surgery because their pain meds are off-limits.
What You Can Do
If you’ve been told you’re allergic to a drug:- Ask: "Was this confirmed with a test?" If not, it’s probably not an allergy.
- Write down what happened: exact symptoms, timing, how long it lasted.
- Don’t assume you’re allergic just because something didn’t feel right. Nausea, fatigue, dizziness, headaches? Almost always side effects.
- Ask your doctor about allergy testing-especially if the drug is important for your treatment.
The Bigger Picture
This isn’t just about individual patients. It’s about smarter healthcare. When we stop mislabeling side effects as allergies, we use better drugs. We reduce antibiotic resistance. We cut costs. We save lives. The data is clear: 90% of people who think they have a drug allergy don’t. And now we have the tools to prove it. The question isn’t whether you can be tested. It’s whether you’ll ask.Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a true penicillin allergy as children lose it over time. Even adults who had a reaction years ago may no longer be allergic. Testing is the only way to know for sure.
If I had a rash from a drug, does that mean I’m allergic?
Not necessarily. Rashes can be side effects, especially with antibiotics like amoxicillin. Up to 10% of people get a non-allergic rash from amoxicillin-even if they’re not allergic. A true allergic rash comes with other symptoms like swelling, itching, or breathing trouble. If it’s just a flat, red rash without other signs, it’s likely not an allergy.
Can I take another drug if I’m allergic to one in the same class?
Maybe. Some drugs in the same class cross-react. For example, if you’re allergic to penicillin, you might also react to amoxicillin or ampicillin. But not always. With sulfa drugs, the risk is higher. But with NSAIDs like ibuprofen and aspirin, cross-reactivity is rare. Always check with a specialist before assuming.
Can a side effect turn into an allergy?
No. A side effect is a pharmacological reaction. An allergy is an immune reaction. They’re different biological pathways. But having one side effect doesn’t mean you’re safe from an allergy-you can have both separately. Just because you got nauseous from a drug doesn’t mean you can’t later develop a true allergic reaction to it.
What should I do if I think I’m allergic to a drug?
Don’t avoid it without confirmation. Write down what happened, when, and how you felt. Then ask your doctor about a referral to an allergist. Skin testing or an oral challenge can give you a clear answer. Don’t let a label from years ago limit your care today.





Posts Comments
Oladeji Omobolaji January 22, 2026 AT 11:27
Man, this hit different. In Nigeria, we just take what the pharmacist gives us and pray. No one even thinks to ask if it's an allergy or just a side effect. I once thought I was allergic to paracetamol because I got dizzy-turns out I was just dehydrated. This post opened my eyes.
Susannah Green January 24, 2026 AT 03:28
So. Many. People. Are. Mislabeling. Side. Effects. As. Allergies. And. It's. Dangerous. Seriously. If you had nausea from metformin? Not allergic. Just adjusting. If you got a rash on amoxicillin? Could be benign. Get tested. Don't assume. Your doctor isn't guessing-your history is.
Kerry Moore January 24, 2026 AT 09:54
This is one of the most clinically significant public health misunderstandings I've encountered in recent years. The data presented-particularly regarding penicillin mislabeling and its downstream consequences on antimicrobial resistance-is not only compelling but also deeply alarming. The economic burden of $1.1 billion annually in the U.S. alone underscores the systemic nature of this issue. I would strongly encourage healthcare institutions to integrate formal allergy clarification protocols into routine medication reconciliation.
Write a comment