Myxedema coma isn't just a rare complication of hypothyroidism-it's a medical emergency that kills up to 60% of people if not treated fast. It doesn't always come with a coma. In fact, the term is being replaced by myxedema crisis in modern medicine because patients don’t need to be unconscious to be in danger. This is a body shutting down, slowly, silently, and often missed until it’s almost too late.
What Happens When Your Thyroid Stops Working
Your thyroid controls your metabolism. When it fails over months or years-often because of Hashimoto’s disease, missed medication, or untreated iodine deficiency-your body starts to slow down. Heart rate drops. Body temperature plummets. Breathing gets shallow. Your brain feels foggy. These aren’t just symptoms of being tired. They’re signs your organs are starving for thyroid hormone. In myxedema crisis, free T4 levels fall below 0.9 ng/dL, and TSH soars past 100 mIU/L. You’ll see hyponatremia (sodium under 135 mmol/L) in 7 out of 10 cases. Your kidneys slow down. Your lungs can’t clear carbon dioxide. You might develop ileus-your gut stops moving. You become cold, slow, and confused. In elderly patients, this looks like depression, dementia, or just "getting old." That’s why so many cases are missed.Who’s at Risk?
Women over 60 are most vulnerable-three times more likely than men. But men don’t escape. In fact, men are more likely to be misdiagnosed because doctors don’t expect hypothyroidism in them. The condition spikes in winter. Cold exposure is a major trigger. A patient who forgets their levothyroxine during a hospital stay for pneumonia? That’s a classic setup. Infections cause 30-50% of cases. Other triggers include heart attacks, strokes, sedatives, and even just being left in a cold room. A 2022 survey of 427 hypothyroid patients found 18% had nearly died from a near-miss event. Half of those were triggered by hospitalizations. One woman spent 11 days in the ICU after stopping her thyroid meds during a pneumonia admission. She’d been told her symptoms were "just depression" for 18 months.How It’s Different From Other Emergencies
Thyroid storm is the opposite-it’s hyperthyroidism on fire. Fast heart rate, high fever, agitation. Myxedema coma is the opposite: slow, cold, quiet. Diabetic ketoacidosis has clear numbers: glucose over 250, pH under 7.3. Myxedema coma doesn’t. You can’t wait for labs. If you see altered mental status, hypothermia (under 35°C), and a known or suspected cause like infection, treat it like a crisis-right now. The mortality rate? 25-60%. That’s higher than diabetic ketoacidosis (2-5%) and close to adrenal crisis. The biggest killer? Delay. Every hour without treatment raises death risk by 10%. The average time to treatment? 6-12 hours. With proper recognition, that drops to under 2 hours.
The Emergency Protocol: Do This Now
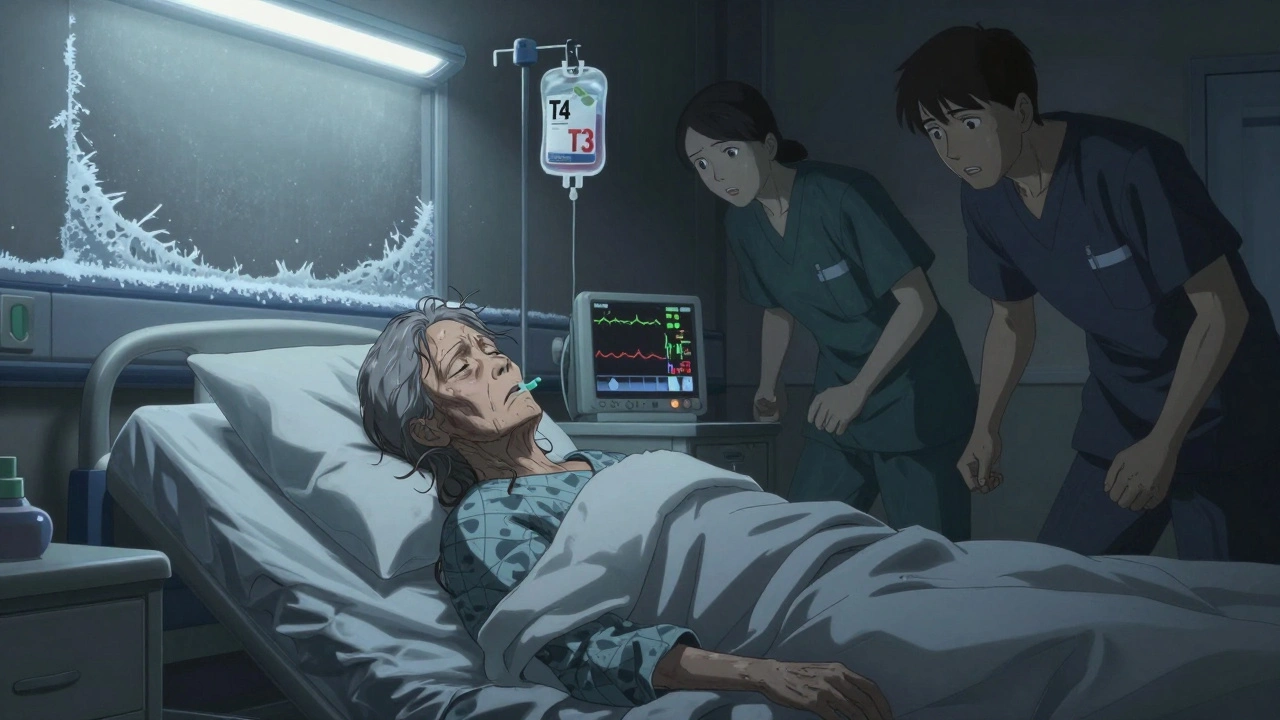
There’s no time to wait for test results. The moment you suspect myxedema crisis, start the protocol:- Secure the airway. Half to 70% of patients need intubation. Breathing is too slow. Oxygen drops. Carbon dioxide builds up. Don’t wait for respiratory arrest.
- Give thyroid hormone immediately. Start with 300-500 mcg of intravenous levothyroxine (T4). In severe cases, especially with heart problems, add 10-20 mcg of liothyronine (T3) every 8 hours. A 2022 Endocrine Society update says T3 should be first-line in cardiac compromise-it cuts 30-day mortality by 15%.
- Rewarm slowly. No heating blankets. No warm IV fluids. Passive rewarming only-cover with blankets, raise room temperature. Active warming can cause heart failure before hormone levels rise.
- Treat the trigger. Assume infection until proven otherwise. Give broad-spectrum antibiotics immediately. Pneumonia and UTIs are the most common culprits. Check for heart attack, stroke, or recent cold exposure using the DIMES mnemonic: Drugs, Infection, Myocardial infarction/CVA, Exposure, Stroke.
- Correct sodium carefully. Hyponatremia is common. But fix it too fast, and you risk osmotic demyelination-a devastating brain injury. Limit correction to 4-6 mmol/L in the first 24 hours.
What Not to Do
Don’t wait for labs. Don’t assume it’s just old age or depression. Don’t give corticosteroids unless adrenal insufficiency is confirmed-many patients have low cortisol because hypothyroidism suppresses the HPA axis. Don’t use active warming. Don’t give sedatives or opioids-they worsen respiratory depression. A 2023 study in Medical News Today found the biggest mistake clinicians make is waiting. One patient died after a 14-hour delay while waiting for thyroid test results. The lab took six hours. The patient didn’t survive.What Recovery Looks Like
If treated fast, improvement can be dramatic. Patients often wake up within 24-48 hours. Mental clarity returns. Body temperature normalizes. Heart rate picks up. But recovery isn’t instant. Full hormone replacement takes weeks. Patients need lifelong thyroid medication and close follow-up. Many survivors report feeling like they’ve been "brought back from the dead." One Reddit user wrote: "I wore three layers in 75°F weather and still shivered. After the IV T4, I took off my sweater in the ICU and didn’t feel cold for the first time in years. It was like someone flipped a switch."
Why This Matters Now
The population is aging. By 2030, myxedema coma cases are expected to rise 20% globally. In developing countries, where thyroid testing is scarce, many cases go undiagnosed until crisis hits. Hospitals in colder regions-Scandinavia, Canada, parts of the U.S.-see higher rates. The Joint Commission now requires emergency departments to have protocols in place. 87% of U.S. hospitals do. But disparities remain. Uninsured patients wait 35% longer for treatment and have 22% higher death rates. This isn’t just a medical issue-it’s a system failure.What You Can Do
If you or someone you know has hypothyroidism:- Never stop thyroid medication without a doctor’s order.
- Keep a list of your meds and doses in your wallet or phone.
- If you get sick-especially with fever, cough, or infection-call your endocrinologist immediately.
- Know the warning signs: extreme cold, confusion, slow speech, low heart rate, swelling in the face or legs.
- If you’re a caregiver, don’t dismiss fatigue or memory issues as "just aging."






Posts Comments
Lauren Scrima December 13, 2025 AT 05:30
So… you’re telling me we’re still letting people die because doctors think it’s just ‘depression’ or ‘getting old’? 😑 I’ve seen this happen. Twice. And no one blinked. Just… sigh and order a CT.
Hamza Laassili December 14, 2025 AT 14:37
AMERICA NEEDS TO STOP IGNORING THYROID ISSUES!! I MEAN COME ON!! WE GOT A PANDEMIC AND PEOPLE ARE STILL FORGETTING THEIR MEDS??!??! THIS ISN’T A DRAMA, IT’S A LIVING NIGHTMARE!!
Constantine Vigderman December 15, 2025 AT 07:45
This is honestly one of the most important posts I’ve read all year 🙏 I had a cousin who nearly died from this and they thought she was just 'lazy.' Now she’s back to hiking, cooking, and yelling at her cats. Life-saving info right here!
Emily Haworth December 16, 2025 AT 23:08
Wait… so if you stop thyroxine, you’re basically signing up for a government experiment? 😳 I’ve heard they’re using hypothyroid patients as test subjects in cold rooms to see how fast they shut down… 🤔 #DeepStateEndo
Tom Zerkoff December 18, 2025 AT 11:16
While the clinical protocol outlined is accurate and evidence-based, I would respectfully suggest that the implicit assumption-that all clinicians are uniformly negligent-is not empirically supported. Many institutions have implemented rapid-response thyroid panels, particularly in geriatric emergency departments.
kevin moranga December 19, 2025 AT 13:36
I work in the ER and let me tell you, this happens way more than people think. We had a guy last winter-72, forgot his meds, came in mumbling, temp 92°F, heart rate 38. We started T4 right away, and by morning he was asking for pancakes. Just… wow. It’s like hitting the reset button on a broken computer. Don’t wait. Don’t overthink. Give the hormone. Save the life.
Alvin Montanez December 20, 2025 AT 07:41
It’s not that hard to understand. If you have a chronic condition and you stop taking your meds, you’re not being ‘stubborn’-you’re being dangerously stupid. And now you want society to pay for your ignorance? No. People need to be held accountable. Your thyroid doesn’t care if you ‘forgot.’ It just shuts down. And then you die. And it’s preventable. That’s not tragedy-it’s negligence.
sharon soila December 21, 2025 AT 23:49
Every life is sacred. And when we fail to see the quiet suffering of the elderly, we fail ourselves. We must act with compassion, not just protocol. A warm blanket, a listening ear, and a hormone replacement-these are not just medical acts. They are acts of love.
Tyrone Marshall December 23, 2025 AT 03:58
Real talk: this isn’t just about thyroid hormones. It’s about how we treat people who are ‘invisible’-older, quiet, tired-looking. We write them off as ‘just aging.’ But aging isn’t a death sentence. It’s a phase. And if we can save someone with a single IV dose, why are we still waiting? We’re not just treating a hormone deficiency-we’re restoring dignity.
Yatendra S December 24, 2025 AT 14:13
Thyroid is the soul’s thermostat. When it fails, the body becomes a ghost of itself. The West ignores this because it cannot quantify suffering. But the East knows: energy flows, and when it stagnates, the body remembers. This is not medicine. This is ancient wisdom wearing a lab coat.
Himmat Singh December 24, 2025 AT 16:30
It is a fallacy to claim that myxedema crisis is underdiagnosed. In fact, the diagnostic criteria have been clearly defined since 1987 by the American Thyroid Association. The real issue is non-compliance and systemic underfunding of endocrine services-not ignorance.
nina nakamura December 26, 2025 AT 15:41
Stop pretending this is a medical mystery. People die because they’re lazy. They stop their meds. They don’t call their doctor. They wait until they’re barely breathing. Then they cry about ‘system failure.’ No. It’s personal failure. And now you want a lecture on protocol? Fix yourself first.
Webster Bull December 27, 2025 AT 16:15
My aunt had this. They thought she had dementia. She didn’t even know her own name. Gave her T4. 12 hours later she asked for pie. And remembered my dog’s name. I’ll never forget it. You don’t need fancy gear. Just know the signs. And act.
Cole Newman December 29, 2025 AT 06:08
Wait so if I’m cold and tired, does that mean I’m in myxedema? I took a nap yesterday. I’m 28. I think I’m dying. Someone send help. Or at least a blanket. And maybe some levothyroxine. I’ll take it. I’m scared now.
Scott Butler December 30, 2025 AT 16:06
This is why we need border control over hormones. People from other countries come here, stop their meds, then blame America for their collapse. We’re not your pharmacy. Take responsibility. And if you’re from a country that doesn’t even test TSH, maybe don’t move here and then act surprised when you almost die.
Write a comment