Bringing a medication action plan to your doctor’s visit isn’t just a formality-it’s one of the most effective ways to prevent dangerous mistakes, avoid hospital visits, and make sure you’re taking your medicines the right way. If you’re on three or more medications, have a chronic condition like diabetes or heart disease, or have ever been confused about what to take and when, this simple paper or digital tool can save your life.
What Exactly Is a Medication Action Plan?
A Medication Action Plan (MAP) is a standardized form that lays out your current medicines, why you’re taking them, what you’re supposed to do, and what to watch out for. It’s not just a list. It’s a living document designed for real conversations between you and your healthcare team. The format used in the U.S. is based on CMS1245776, the official template required for Medicare Part D Medication Therapy Management programs. In Germany, a nearly identical system called the Medication Plan has been mandatory since 2016 for anyone taking three or more prescribed drugs.What makes it different from a simple pill list? It includes specific action steps, space to track what you actually did, and prompts for questions you might forget to ask. Studies show that patients using a properly completed MAP are 87.5% more likely to find critical information about their meds on the first try-and medication errors drop by up to 23%.
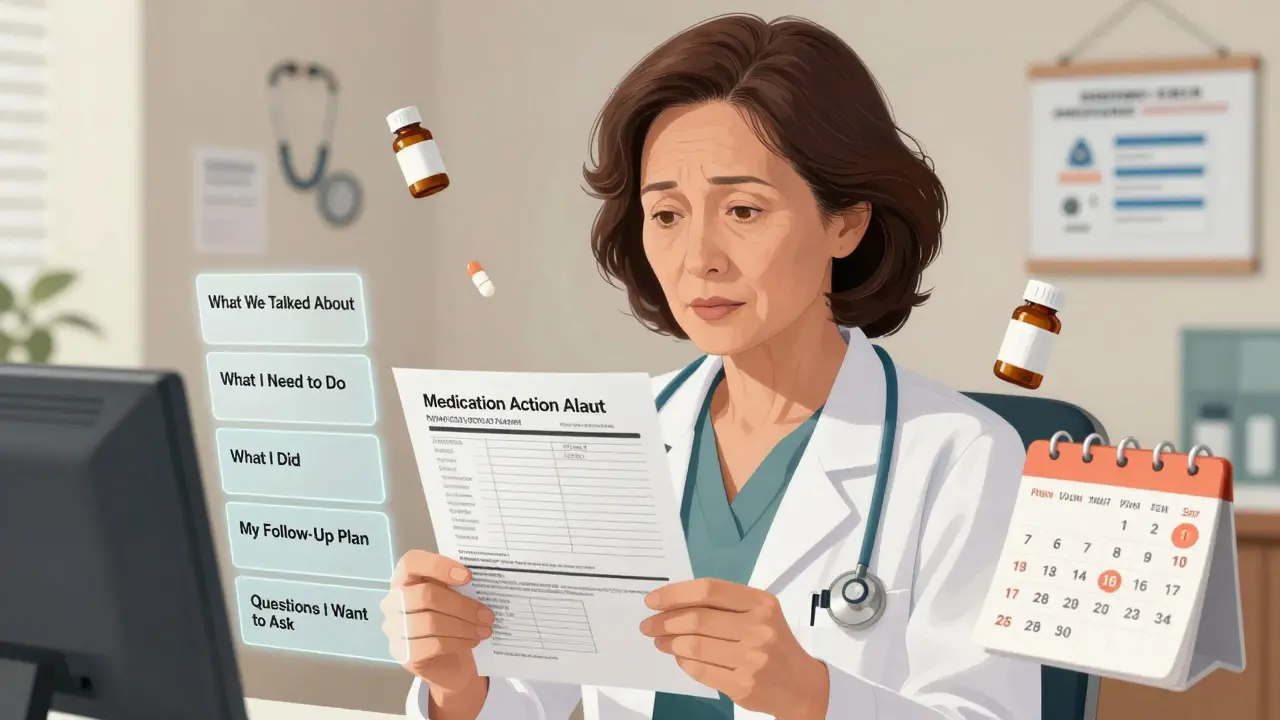
What Should Be in Your Medication Action Plan?
A good MAP has five non-negotiable sections. If your form doesn’t have these, ask your pharmacist or doctor for the official version:- What we talked about: A summary of the visit-new diagnoses, changes in symptoms, or concerns raised.
- What I need to do: Clear, specific instructions like “Take metformin 500mg with breakfast and dinner starting tomorrow,” not “Take as directed.” Research shows specific instructions lead to 34% better adherence.
- What I did and when I did it: A daily or weekly tracker where you mark whether you took your pills. This is where pharmacists spend an average of 3.7 minutes per visit, looking for patterns like missed doses or double-dosing.
- My follow-up plan: Dates for next appointments, lab tests, or when to call your provider. Include symptoms that mean you should act-like “If my blood pressure is above 160/90, call the clinic.”
- Questions I want to ask: Write these down before you walk in. People who do this are far more likely to get their concerns addressed.
Every template must also include your full name, date the plan was created, your provider’s contact info, and the exact start and stop dates for every medication-not just the month. CMS requires the precise date of discontinuation to prevent dangerous overlaps.
How to Prepare Before Your Visit
Don’t show up with a half-filled form. Come ready:- Bring every pill bottle-even the empty ones. Studies show this improves accuracy by 37.2% compared to just describing your meds from memory.
- Cross out discontinued meds with the exact date you stopped and why (e.g., “Stopped lisinopril on 1/5/2026-caused cough”).
- Write down new meds you’ve started since your last visit, including over-the-counter drugs, vitamins, or herbal supplements.
- Check your tracker. Did you miss any doses? Were there side effects? Note them clearly.
- Fill out your questions. Don’t rely on your memory. Write: “Why am I on this blood thinner?” or “Can I stop the sleeping pill?”
Many patients lose their MAPs or forget to update them. A common fix? Keep a laminated wallet-sized copy. It fits in your purse, wallet, or even your phone case. About 80% of older adults who use this method keep it with them consistently.

What Happens During the Visit
Your provider should spend the first 5 to 7 minutes reviewing your MAP. Here’s how it should go:- They’ll cross-reference your pill bottles with the list. If something doesn’t match, they’ll ask why.
- They’ll look at your “What I did” section. If you’ve missed doses, they won’t just scold you-they’ll ask what got in the way. Was it cost? Side effects? Confusion?
- They’ll update the plan right there. If you’re starting a new drug, they’ll write the name, dose, time, and reason. If you’re stopping one, they’ll write the exact date.
- They’ll check for high-risk meds-like sleeping pills or blood thinners-that increase fall risk in older adults. This review takes 8 to 12 minutes per visit.
- They’ll use the “Questions I want to ask” section to make sure nothing gets left out.
Don’t let them rush through this. If they skip the MAP, say: “I brought this to make sure we don’t miss anything. Can we go through it together?”
After the Visit: Keep It Alive
Your MAP isn’t done when you leave the office. Here’s what to do next:- Update your copy. If your provider made changes, write them in immediately. Don’t wait.
- Give a copy to your caregiver. A family member, partner, or friend should have the same version. In emergencies, they’ll know exactly what you’re taking.
- Bring it to every appointment-even if it’s for your knee pain or a cold. Medication interactions don’t care what your reason is for being there.
- Take it to the ER. The CDC specifically recommends this. If you’re admitted, the ER team will check your MAP first to avoid dangerous drug clashes.
Patients who share their MAP with multiple providers have 22.8% fewer duplicate prescriptions. That’s not just convenience-it’s safety.
Common Mistakes (And How to Avoid Them)
Even with the best intentions, people mess up. Here are the top errors-and how to dodge them:- Not writing stop dates: This is the #1 error. If you stop a drug, write the exact date. Without it, your next doctor might restart it-dangerous if it caused side effects before.
- Using vague language: “Take as directed” is useless. Always specify time, dose, and reason.
- Ignoring OTC meds: Aspirin, ibuprofen, sleep aids, and even herbal supplements like St. John’s Wort can interact with prescriptions. List them all.
- Letting it sit: If you don’t update it between visits, it becomes a paperweight. Treat it like a living document.
- Not teaching patients how to use it: One study found that when pharmacists spent 5+ minutes teaching patients how to track doses, 78.4% updated their plan correctly before the next visit. Without teaching, only 32.1% did.
Why This Matters More Than You Think
The stakes are high. In the U.S., medication errors send over 1.3 million people to the ER every year. The Agency for Healthcare Research and Quality says medication reconciliation-using tools like the MAP-is one of the top 11 proven ways to improve patient safety.Dr. Jerry Fahrni of the National Association of Chain Drug Stores says: “The single most effective intervention in reducing medication-related hospitalizations is the consistent use of a standardized Medication Action Plan during every provider encounter.”
And it’s not just for seniors. People of all ages on multiple meds benefit. A 42-year-old with asthma, depression, and high blood pressure? Same rules apply. A teenager on ADHD meds and antibiotics? They need this too.
The system isn’t perfect. Some clinics still don’t have electronic systems that sync with MAPs. Health literacy is a barrier-only 12% of U.S. adults have proficient health literacy, according to the National Assessment of Adult Literacy. That’s why simple language, big fonts, and visual checkmarks matter.
But the data is clear: when used right, this tool works. It catches dangerous combinations. It prevents overdoses. It gives you control.
Real Stories
Mary Thompson, 68, from Ohio, says: “When I started bringing my MAP to every appointment and asking my doctors to update it, my cardiologist caught that I was taking two blood pressure medications that shouldn’t be combined. That stopped a potential hospitalization.”On Reddit, pharmacist John Davis from North Carolina shares: “Many elderly patients lose their MAPs or don’t understand how to update them. We now give them laminated cards with just the essentials. It’s changed everything.”
These aren’t rare cases. They’re the rule when people take a few minutes to use the tool properly.
Where to Get a Template
You don’t need to buy one. The CDC offers a free, printable MyMedications Action Plan (2021 version) online. Pharmacies like CVS and Walgreens often have them at the front desk. Medicare beneficiaries can request the official CMS version from their Part D plan. If you’re unsure, ask your pharmacist-they’re required to provide one at no cost.And if your provider doesn’t use one? Bring your own. They’ll be glad you did.
Do I need a Medication Action Plan if I only take one or two medications?
You still benefit, especially if you’re taking any high-risk drugs like blood thinners, diabetes meds, or sleeping pills. Even two medications can interact. The MAP helps you track side effects and remember why you’re taking each one. It’s not just for people on five or more drugs-it’s for anyone who wants to avoid mistakes.
Can I use a digital app instead of a paper template?
Yes, but make sure the app lets you print a clear, updated version for your provider. Many apps don’t show stop dates or reasons for changes. The CDC’s printable template is designed for easy sharing. If you use an app, always bring a printed copy to your visit-providers still rely on paper during appointments.
What if my doctor doesn’t want to use the Medication Action Plan?
Politely insist. Say: “I brought this to make sure we don’t miss anything important.” Studies show that 89.7% of pharmacists and 62.4% of primary care clinics use some form of MAP. Your provider may not be familiar with it, but they’re trained to use tools that improve safety. If they refuse, ask for a referral to a pharmacist who specializes in medication management.
How often should I update my Medication Action Plan?
Every time you see any healthcare provider-even for a cold or a checkup. Changes happen fast: a new prescription, a discontinued drug, a side effect. Treat it like your wallet-update it after every change. The American College of Clinical Pharmacy calls it a “living document,” not a one-time form.
Is the Medication Action Plan covered by insurance?
Yes-if you’re on Medicare Part D, the plan is required as part of your Medication Therapy Management services. Most private insurers cover it too, especially if you have multiple chronic conditions. Pharmacists can bill for time spent reviewing and updating your MAP. If you’re asked to pay for it, ask if your insurer covers MTM services. You shouldn’t have to pay out of pocket.






Posts Comments
Sonal Guha January 11, 2026 AT 23:25
MAPs are overrated
gary ysturiz January 12, 2026 AT 20:36
This is exactly the kind of practical tool that saves lives. I’ve seen grandparents forget their meds or mix up pills-this simple plan cuts through the chaos. No fluff, just clarity. Everyone on multiple meds should use this, no exceptions.
Jessica Bnouzalim January 13, 2026 AT 22:52
I love this so much!! I gave my mom a laminated copy after she nearly ended up in the ER because she took two blood pressure pills by accident-she’s been carrying it in her purse ever since. Also, writing down questions before the appointment? Game changer. I used to walk out feeling like I forgot half the stuff I wanted to ask. Now I just point to my list and boom-done.
Audu ikhlas January 15, 2026 AT 14:56
Why are we letting Americans dictate healthcare norms? In Nigeria, we don’t need fancy templates-our elders just remember what they need, or they die. This is over-medicalized nonsense. Who has time to fill out forms when you’re trying to survive? This is Western bureaucracy dressed up as care.
Alice Elanora Shepherd January 15, 2026 AT 20:21
As a pharmacist, I’ve seen this work-repeatedly. But the real issue? Most providers don’t know how to use it. They glance at it, then move on. The template is perfect-but it’s useless unless the clinician engages with it. I train my staff to ask: ‘What’s the most confusing part here?’ before even looking at the meds. That’s when real change happens.
Sumit Sharma January 17, 2026 AT 15:29
There’s a critical gap in implementation: pharmacists are the only ones consistently using MAPs. Primary care physicians still rely on outdated electronic records that don’t sync with patient-generated plans. The CDC template is evidence-based, but without interoperability with EHRs, it’s a paper exercise. We need API integration-not just laminated cards.
Jay Powers January 18, 2026 AT 14:36
I used to think this was for old people until my sister, 31, got on three new meds for anxiety, thyroid, and migraines. She was overwhelmed. We printed the CDC template together. Now she checks it every morning. She says it’s the first thing that made her feel like she wasn’t just a patient number. This isn’t bureaucracy-it’s dignity.
Lawrence Jung January 19, 2026 AT 11:34
People think this is about safety but it’s really about control. Who gave the government the right to tell us how to manage our own bodies? The MAP is a tool of compliance disguised as empowerment. You think you’re in charge but you’re just following someone else’s checklist. True autonomy means trusting your intuition-not a printed form.
laura manning January 21, 2026 AT 03:33
According to the Agency for Healthcare Research and Quality (AHRQ), medication reconciliation via standardized templates reduces adverse drug events by 23% (AHRQ Publication No. 19-0028-EF, 2019). Furthermore, the CMS1245776 template, as referenced, aligns with the 2021 Medicare Part D MTM requirements. Non-compliance with precise stop dates, as noted, constitutes a Class II medical error under FDA guidance. Therefore, failure to implement this protocol may constitute negligence in clinical practice.
TiM Vince January 22, 2026 AT 17:45
I’m from the U.S. and I’ve traveled to 12 countries. In India, Brazil, Ghana, and Japan-I saw people using handwritten lists, phone notes, even sticky notes. But the ones who survived longest? The ones who had a clear, simple, updated plan. It’s not about being American. It’s about being smart. This isn’t a luxury. It’s a lifeline. I carry mine in my wallet. Always.
Write a comment