When you take a generic drug, you expect it to work just like the brand-name version. But what happens when it doesn’t? What if you feel worse, or the medication just doesn’t seem to help anymore? That’s where MedWatch comes in - the U.S. Food and Drug Administration’s system for collecting real-world safety data on all medications, including generics.
Generics make up about 90% of all prescriptions filled in the U.S. They’re cheaper, widely available, and approved by the FDA as bioequivalent to their brand-name counterparts. But bioequivalence doesn’t always mean identical experience. Differences in inactive ingredients, manufacturing processes, or even how the pill breaks down in your body can lead to real problems - and those problems need to be tracked.
How MedWatch Works for Generic Drugs
MedWatch isn’t a law. It’s a voluntary system. That means doctors, pharmacists, patients, and drug manufacturers can report problems - but they don’t have to. Still, it’s the main way the FDA learns about unexpected side effects, allergic reactions, or when a generic drug just doesn’t seem to work as well as it should.
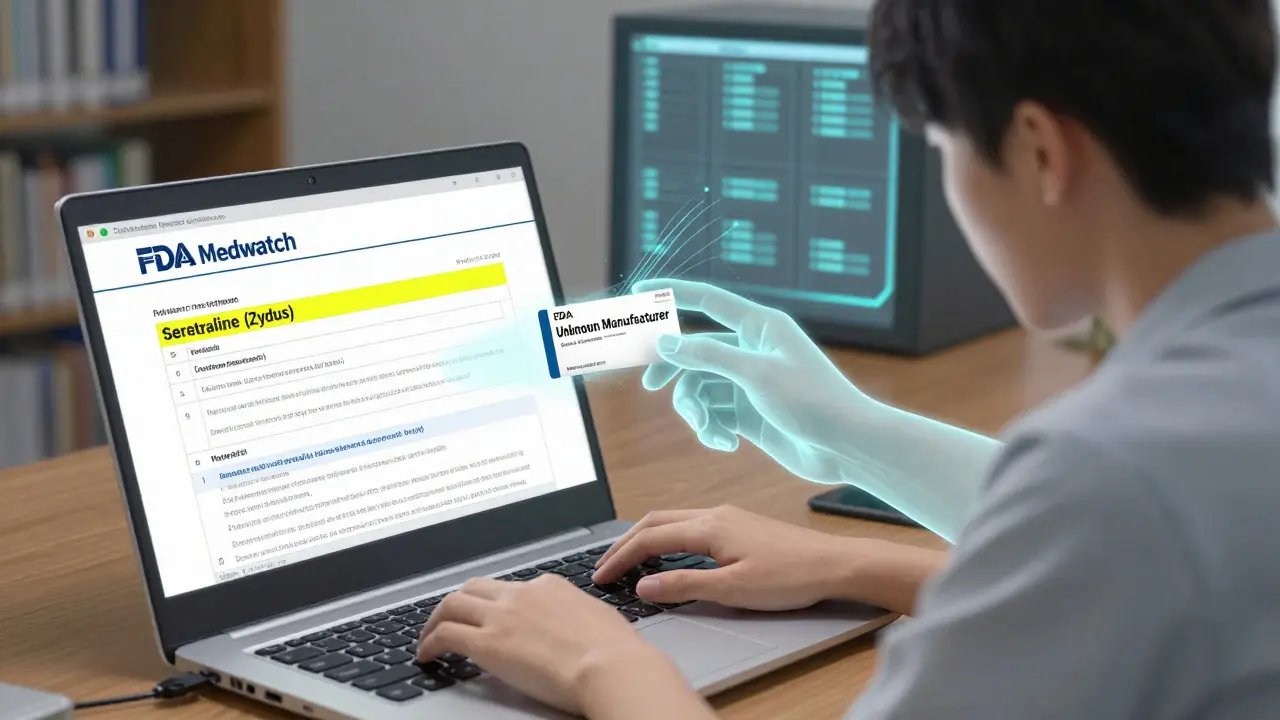
When someone reports an issue, they fill out Form FDA 3500 - either online at www.fda.gov/MedWatch or on paper. The form asks for basic info: what drug was taken, what happened, when it happened, and who reported it. For generics, the key detail is this: you need to say which generic it was. Not just “sertraline.” Not just “levothyroxine.” You need to include the manufacturer’s name if you know it - like Mylan, Teva, or Sandoz.
Why? Because not all generics are made the same. Two pills with the same active ingredient can behave differently in your body. One might have a coating that dissolves slower. Another might use a different filler that triggers a reaction. If you just report “generic sertraline,” the FDA can’t tell which company made the bad batch. And without that, they can’t fix it.
The Data Gap: Why Generic Reports Are Hard to Track
Here’s the problem: most people don’t know which manufacturer made their generic pill. Pharmacists often switch brands without telling patients. Insurance plans push the cheapest option. So when someone reports a problem, they often write “generic” and leave it at that.
According to FDA data from 2020 to 2024, only 32.7% of reports involving generics included the manufacturer name. Compare that to brand-name drugs - 89.4% of those reports named the exact company. That’s a huge gap. And it makes it nearly impossible to spot patterns. If 100 people report dizziness after taking a generic bupropion, but none say it was made by Mylan, the FDA can’t investigate Mylan specifically. They see a general “bupropion” signal - and that’s not enough.
Researchers have tried to fix this. In 2022, a team developed an algorithm to automatically detect which generic drugs were involved in reports by cross-referencing names, NDC codes, and manufacturer details. By early 2024, this tool was fully integrated into the FDA’s Adverse Event Reporting System (FAERS). It now identifies generics with 92.4% accuracy. That’s a big step forward. But it still can’t catch every report where the manufacturer was left blank.
What Gets Reported - And What Doesn’t
Most reports about generics fall into one of three categories:
- Therapeutic failure: The drug just doesn’t work. A patient who switched from brand-name levothyroxine to a generic might suddenly feel exhausted, gain weight, or have trouble concentrating - even though their lab numbers look fine.
- Unexpected side effects: New or worse side effects after switching. Someone might start having headaches, nausea, or anxiety after changing to a different generic version of sertraline.
- Product quality issues: Pills that crumble, have odd colors, or don’t dissolve properly. One patient reported a generic metformin tablet that looked like it had chalky streaks. Turns out, it was a bad batch.
But here’s the catch: many of these issues never get reported. Patients assume it’s their condition worsening, not the drug. Doctors don’t always ask about recent switches. Pharmacists are busy. And even when reports are made, they often lack the critical details needed to trigger action.
Real Cases That Made a Difference
There are success stories. In 2022, multiple MedWatch reports came in about a specific generic version of bupropion XL made by Mylan. Patients described sudden mood swings, panic attacks, and loss of effectiveness - symptoms they hadn’t had on the brand-name version. The FDA reviewed the reports, flagged the pattern, and launched an investigation. Within 11 months, Mylan changed the formulation and updated the product label to warn about possible variability in absorption.
Another case involved a generic version of levothyroxine. Over 40 reports from patients across 12 states described inconsistent energy levels and heart palpitations. The FDA contacted the manufacturer, who tested their batches and found a slight variation in dissolution rates. They adjusted their manufacturing process and notified prescribers.
These cases didn’t happen by accident. They happened because someone - a patient, a pharmacist, a doctor - took the time to report it. And they included the manufacturer name.
How to Report a Problem With a Generic Drug
If you suspect a generic drug isn’t working right, here’s how to report it - and how to make sure your report actually helps:
- Check the label. Look at the pill bottle. Find the National Drug Code (NDC) number. It’s usually a 10- or 11-digit number. Write it down.
- Identify the manufacturer. The label should say who made it - like “Teva Pharmaceuticals” or “Actavis.” If not, look up the NDC online using the FDA’s NDC Directory.
- Go to MedWatch. Visit www.fda.gov/MedWatch and click “Report a Problem.”
- Fill out the form. In the drug name field, type: [Generic name] (manufacturer name). Example: “Levothyroxine (Teva)” or “Sertraline (Zydus)”.
- Be specific. Describe what happened. When did it start? Did you switch from another version? Did labs change? Include dates and symptoms.
- Submit. You don’t need to give your name, but including your contact info lets the FDA follow up if they need more details.
Pro tip: Keep the pill bottle until you’re sure the issue is resolved. If you need to report again later, you’ll need the NDC and manufacturer info.
Why This Matters - And Why It’s Still Broken
Generics save the U.S. healthcare system over $300 billion a year. But safety can’t be an afterthought. The FDA estimates that 45-50% of all adverse event reports involve generic drugs. Yet, only 4.7% of those reports mention “generic” in the context of therapeutic failure. That means most problems go unnoticed.
The system isn’t broken - it’s underused. The tools are there. The algorithm works. The forms are simple. But without clear, detailed reports, the FDA can’t act. And without action, bad batches keep circulating. Patients keep suffering. And the trust in generics - already fragile for some - erodes further.
Healthcare providers have an important role too. When a patient says, “This generic doesn’t feel right,” don’t dismiss it. Ask: Which brand? Do you still have the bottle? Write down the NDC. Submit the report. It takes five minutes. It might save someone else from the same problem.
And if you’re a patient? Don’t assume it’s all in your head. If you notice a change after switching to a new generic - especially if it’s worse than before - speak up. Your report matters. It’s the only way the FDA finds out when something’s wrong.
What’s Next for Generic Drug Safety
The FDA is working on bigger changes. By 2026, they plan to connect MedWatch directly with electronic health records. That means when a doctor prescribes a generic, the system could auto-fill the manufacturer and NDC code - no guesswork needed. It’s a game-changer.
Meanwhile, the Generic Drug User Fee Amendments (GDUFA) III plan, launched in 2023, commits the FDA to improving how it tracks and evaluates generic drug safety. More training for pharmacists. Better consumer materials in Spanish and other languages. And a push to make reporting easier on mobile devices.
But none of this will fix the core issue: people still don’t know how to report properly. Until we change that, the system will keep missing signals - and the safest, cheapest drugs in the country will remain the least understood.