Fluoroquinolone Delirium Risk Calculator
This tool helps assess your risk of developing fluoroquinolone-induced delirium based on key factors mentioned in the article. Note: This is not medical advice.
Important Note: If you or a loved one is experiencing confusion or hallucinations while taking fluoroquinolones, stop the medication immediately and contact a healthcare provider. Symptoms often resolve within 48-96 hours after discontinuation.
Every year, millions of older adults are prescribed fluoroquinolones for common infections like urinary tract infections or pneumonia. These antibiotics-like levofloxacin, ciprofloxacin, and moxifloxacin-work fast and are often seen as a go-to choice. But behind the convenience lies a hidden risk: sudden, terrifying confusion that can look like dementia, but isn’t. This is fluoroquinolone-induced delirium, and it’s more common in seniors than most doctors realize.
What Exactly Is Fluoroquinolone-Induced Delirium?
Delirium isn’t just being forgetful. It’s a sudden, sharp drop in mental clarity that can turn a person into someone unrecognizable. Imagine your parent or grandparent, usually sharp and oriented, suddenly not knowing where they are, seeing things that aren’t there, or becoming intensely agitated. That’s delirium. And for older adults on fluoroquinolones, it can happen within just 1 to 3 days of starting the drug.The symptoms are unmistakable: confusion about time or place, hallucinations (seeing shadows or hearing voices), inability to focus, rapid mood swings, and memory gaps. These aren’t signs of aging or dementia-they’re signs of a drug reaction. The good news? When caught early and the antibiotic is stopped, most people bounce back fully within 48 to 96 hours. But if missed, the consequences can be long-lasting: longer hospital stays, increased risk of nursing home placement, and even higher death rates.
Why Do Fluoroquinolones Affect the Brain?
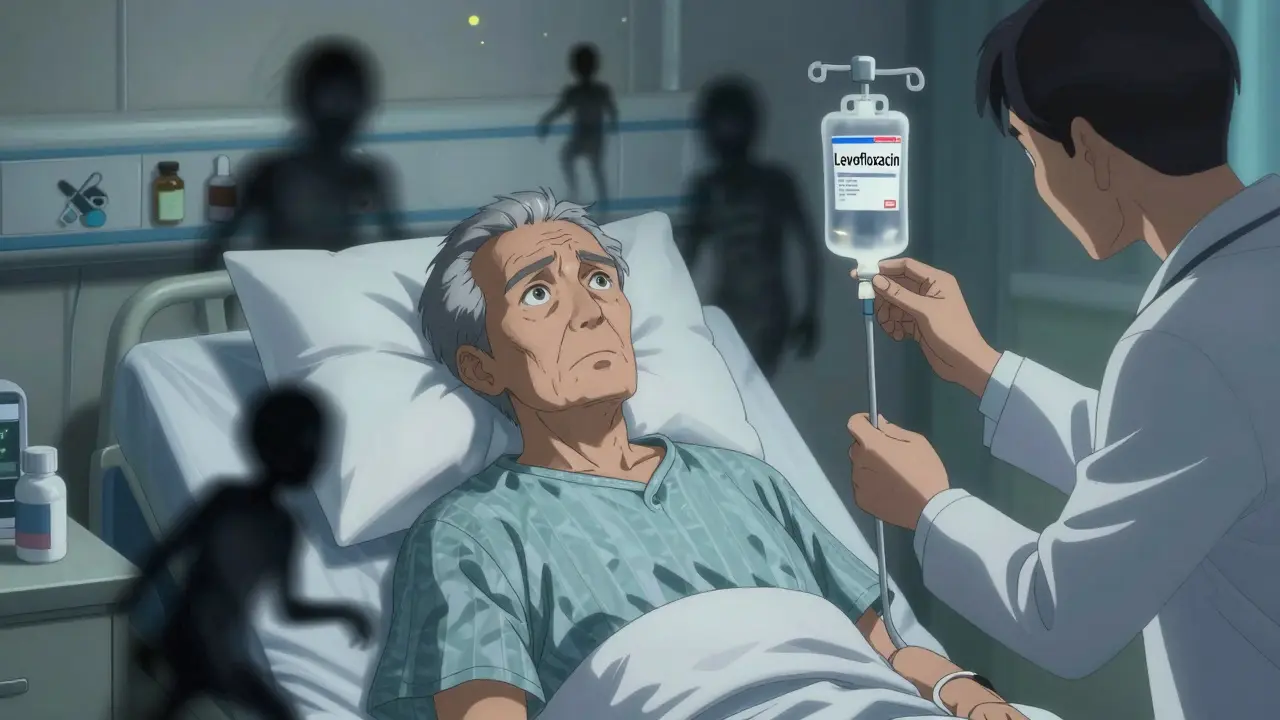
Fluoroquinolones aren’t just killing bacteria-they’re also messing with your brain chemistry. Their main target is bacterial enzymes, but they accidentally interfere with human brain receptors too. Specifically, they block GABA-A receptors, which are the brain’s natural brakes. When those brakes fail, brain activity goes into overdrive. This imbalance triggers excitotoxicity, a process where nerve cells become overstimulated and damaged.Some fluoroquinolones also directly activate NMDA receptors, which are linked to memory and learning. When these receptors are overstimulated, they can cause confusion and hallucinations. This isn’t just theory-it’s been shown in lab studies and confirmed in real patient cases. The more the drug gets into the brain, the worse the reaction. Drugs like levofloxacin and ciprofloxacin penetrate the blood-brain barrier more easily than others, making them riskier, especially in older adults whose barriers are already more permeable.
Who’s Most at Risk?
Not everyone who takes a fluoroquinolone gets delirium. But certain people are far more vulnerable. The biggest risk factor is age. People over 65 make up about 40% of hospitalized adults, and nearly half of all hospital spending in the U.S. goes toward this group. Their bodies process drugs differently: kidneys slow down, liver function declines, and brain chemistry becomes more sensitive.Renal impairment is another major red flag. About 85% of levofloxacin leaves the body through the kidneys. If kidneys aren’t working well, the drug builds up. A dose that’s safe for a 30-year-old can become toxic for a 75-year-old with even mild kidney trouble. Other risk factors include pre-existing dementia or brain injury, dehydration, electrolyte imbalances, and taking multiple medications that affect the nervous system.
Even the dose matters. Studies show that 750 mg daily of levofloxacin carries a higher risk than 500 mg. Yet, many doctors still default to the higher dose for “better coverage,” unaware they’re increasing the chance of a psychiatric emergency.
How Common Is This Really?
You might think this is rare-and technically, it is. Only about 0.5% of people taking fluoroquinolones report neuropsychiatric side effects. But that number is misleading. Most cases go unreported or misdiagnosed. A patient gets confused in the hospital? Staff assume it’s dementia, infection-related delirium, or just “getting old.”When researchers looked back at 391 cases of antibiotic-induced delirium across decades, fluoroquinolones were responsible for nearly 18% of them-the highest of any antibiotic class. In one study, a single hospital found that 1 in 5 cases of sudden delirium in elderly patients on antibiotics was tied to fluoroquinolones. And in community settings, doctors on forums like Reddit report seeing 1 to 3 cases every few years-each time, it took 1 to 2 days to connect the dots.
What Does the FDA Say?
In July 2018, the FDA issued a stark warning: fluoroquinolones can cause serious disturbances in attention, memory, and mental abilities-including delirium. They required drug labels to be updated to include these risks explicitly. The agency also emphasized that these drugs should be reserved for infections with no safer alternatives, especially in older adults.Before that, the risks were buried in fine print. Now, the message is clear: fluoroquinolones aren’t just another antibiotic. They’re a high-risk option for seniors. Since the warning, prescriptions for older adults dropped by over 20%. Hospitals like UCSF cut levofloxacin use for UTIs in seniors by 35% after implementing new protocols.
How Is It Diagnosed?
Diagnosing fluoroquinolone-induced delirium isn’t about one test. It’s about ruling everything else out. Doctors use the DSM-IV criteria: sudden onset, fluctuating symptoms, trouble paying attention, and either disorganized thinking or altered consciousness. Blood tests check for infection, electrolytes, and kidney function. Brain scans (CT or MRI) rule out stroke or tumors. EEGs often come back normal, which helps distinguish it from seizures or epilepsy.The key clue? Timing. Symptoms start within days of beginning the antibiotic. And if you stop the drug, symptoms fade. That’s the diagnostic gold standard. If a patient improves 48 hours after stopping levofloxacin, it’s almost certainly the drug.
What Should Doctors Do Instead?
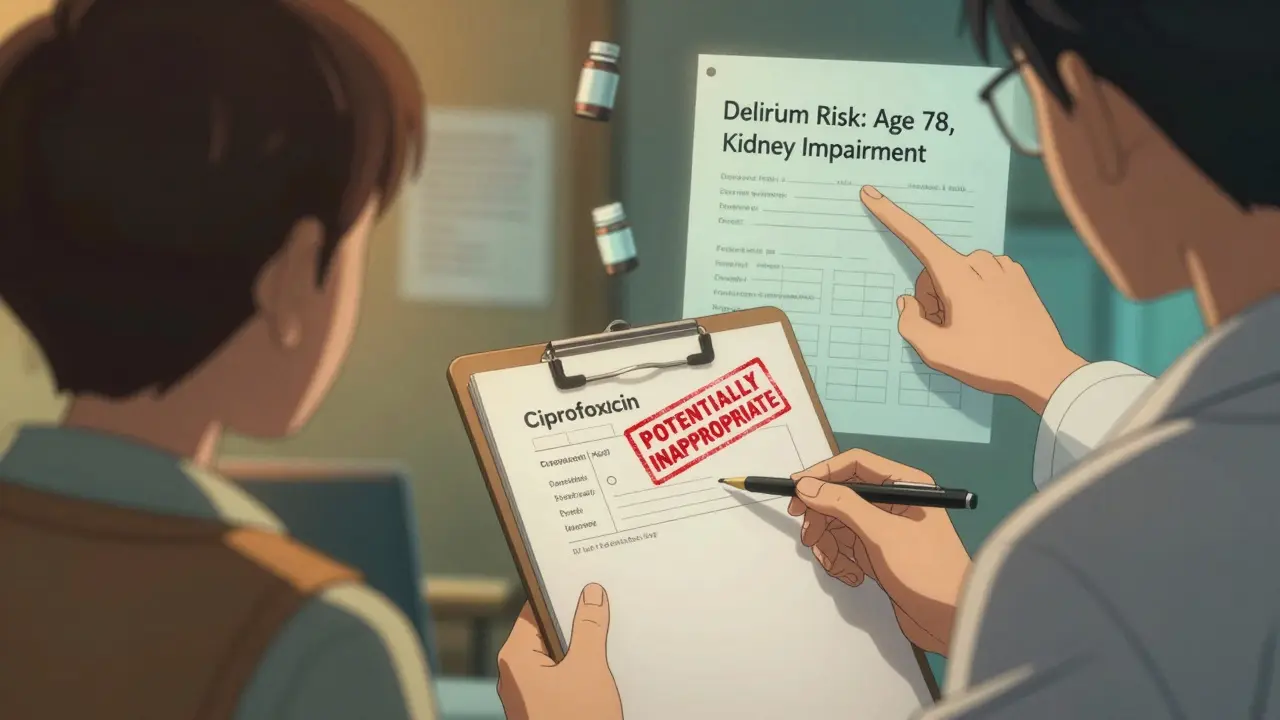
The good news? There are safer alternatives. For urinary tract infections, nitrofurantoin or fosfomycin are preferred in older adults. For pneumonia, amoxicillin-clavulanate or respiratory fluoroquinolone alternatives like azithromycin (with caution) are often better choices. Beta-lactams like penicillins and cephalosporins have much lower brain penetration and rarely cause delirium.There are exceptions, of course. For severe infections like complicated pyelonephritis or resistant pneumonia, fluoroquinolones may still be necessary. But they shouldn’t be the first choice. The American Geriatrics Society’s 2023 Beers Criteria lists fluoroquinolones as “potentially inappropriate” for seniors due to delirium risk. That’s not a suggestion-it’s a guideline backed by decades of evidence.
What Can Families and Caregivers Do?
If your loved one is prescribed a fluoroquinolone, ask: “Is this the safest option?” and “What are the signs of confusion I should watch for?” Pay attention in the first 72 hours. Is your parent suddenly restless? Are they seeing things? Do they forget why they walked into a room? These aren’t “just being old.” They’re warning signs.If you suspect delirium, don’t wait. Call the doctor immediately. Say: “They started this antibiotic three days ago and now they’re hallucinating and confused. Could this be a reaction?” Don’t let them brush it off. The sooner the drug is stopped, the faster recovery happens.
Also, keep a list of all medications-prescription, over-the-counter, supplements. Many seniors take 5 to 10 drugs a day. Some interact with fluoroquinolones and increase brain toxicity. A pharmacist can help spot these.
What’s the Future?
Research is moving in two directions. One: finding biomarkers that predict who’s likely to react. A 2023 study on metronidazole used large data sets to predict who developed brain side effects-similar methods could be applied to fluoroquinolones. Two: designing new versions of these antibiotics that don’t cross the blood-brain barrier. Early lab compounds show promise.Meanwhile, hospitals are adding clinical decision support tools. When a doctor tries to prescribe levofloxacin to a 78-year-old with kidney disease, the system pops up a warning: “High risk for delirium. Consider alternatives.” These tools are saving lives.
But the biggest change is cultural. More doctors are learning to see delirium not as inevitable aging, but as a medical emergency. And more families are speaking up. The days of automatically reaching for fluoroquinolones are ending. Safer choices exist. And for older adults, avoiding unnecessary brain toxicity isn’t just wise-it’s essential.





Posts Comments
Chris porto December 18, 2025 AT 10:51
It's wild how we treat older folks like they're just supposed to fade away. If a drug makes someone hallucinate and forget their own name, maybe we shouldn't be giving it out like candy. I've seen it happen-grandpa thought the TV was talking to him. Turned out it was the antibiotic. He was back to normal in two days after they stopped it. Why is this still not common knowledge?
Allison Pannabekcer December 20, 2025 AT 06:36
This is exactly why we need better education for doctors-and for families. My mom was on cipro for a UTI and became completely unrecognizable. The ER doctor said, 'Oh, she's just confused from the infection.' But it wasn't the infection-it was the drug. We had to push hard to get them to stop it. Once they did, she came back. It's not dementia. It's preventable. We need to stop normalizing this.
Sarah McQuillan December 20, 2025 AT 15:56
Look, I get it. But you're ignoring the fact that these drugs save lives. If you don't want to use them, fine. But don't act like every older person who gets confused is a victim of Big Pharma. Sometimes people just get sick. And sometimes, when you're fighting a life-threatening infection, you need the strong stuff. Stop being so afraid of medicine.
Dorine Anthony December 21, 2025 AT 07:37
My aunt had this happen last year. We didn't know what was going on until the pharmacist mentioned it. She was on levofloxacin for a chest infection. Started acting weird on day two. We called the doctor, they pulled the script, and by day four she was herself again. It's scary how fast it happens. And how few doctors even mention it.
William Liu December 21, 2025 AT 16:17
There's hope. More hospitals are changing their protocols. My sister works in geriatrics and said their new system flags fluoroquinolones for seniors automatically. It's slow, but it's moving in the right direction. We just need to keep pushing. Safer options exist. We just have to choose them.
Frank Drewery December 23, 2025 AT 05:58
I’ve worked in nursing homes for 15 years. This happens more than you think. We call it 'sudden confusion' and chalk it up to age. But after reading this, I realize how many of those cases were probably drug-induced. We need better training. Not just for doctors, but for aides too. They’re the ones who notice the changes first.
mary lizardo December 25, 2025 AT 00:11
The author's argument is structurally unsound. The term 'delirium' is a clinical diagnosis requiring DSM-5 criteria, yet the piece conflates anecdotal reports with epidemiological data. Furthermore, the FDA warning was not a ban, but a risk mitigation notice. To imply that fluoroquinolones are inherently dangerous for elderly patients without accounting for comorbidities, polypharmacy, and renal function is misleading. This is fearmongering dressed as public health advocacy.
jessica . December 25, 2025 AT 20:02
they dont want you to know this but the fda and big pharma are in bed together. these drugs are designed to mess with your mind so youll need more meds later. its all about control. look at the side effects they list-confusion, hallucinations-thats not a bug, its a feature. they want old people dependent. and dont even get me started on the blood brain barrier thing-science is fake anyway
Ryan van Leent December 26, 2025 AT 14:17
why do people always blame the drug and not the patient? my grandpa was 80 and still took his meds wrong. he mixed up his pills. he got confused because he was a mess not because of cipro. stop making everything someone elses fault. also why are we letting doctors be scared of prescribing anything anymore
Sajith Shams December 27, 2025 AT 09:45
As a medical researcher in India, I've seen this repeatedly. Fluoroquinolones are overprescribed everywhere, but in the US, the problem is worse because of profit-driven medicine. Elderly patients are not given proper renal function tests before prescribing. In our hospitals, we check creatinine clearance first. Simple. But in the U.S., it's easier to write a script than to think. This is systemic negligence.
Adrienne Dagg December 29, 2025 AT 04:29
OMG this is so real 😭 my grandma had the same thing. She started seeing spiders on the walls. We thought it was dementia. Turns out it was the antibiotic. She cried for days because she didn’t know who we were. When they stopped it? She hugged us like she’d been gone for years. Please, if you’re reading this-ask your doctor. Don’t wait.
Erica Vest December 31, 2025 AT 03:47
It's worth noting that fluoroquinolone-induced delirium is dose-dependent and reversible, which is why early recognition is critical. The key is clinical suspicion. If a patient over 65 develops acute confusion within 72 hours of starting a fluoroquinolone, the drug is the prime suspect until proven otherwise. Always check renal function, review concomitant medications, and consider alternatives like beta-lactams. This isn't speculation-it's standard geriatric pharmacology.
Chris Davidson December 31, 2025 AT 15:30
Doctors are lazy. They pick the easiest antibiotic because they’re rushed. They don’t think about the brain. They think about the bacteria. But the brain matters too. We need to stop treating elderly patients like they’re disposable. This isn’t just about one drug. It’s about how we value older people in medicine.
Kinnaird Lynsey January 1, 2026 AT 00:48
Interesting how the article says 'safer alternatives exist' but doesn’t mention that those alternatives often require longer courses or IV administration. So yes, nitrofurantoin is safer-but it takes 7 days. And if you’re in a nursing home with no IV access? What then? The system is broken, not just the drug.
Andrew Kelly January 2, 2026 AT 17:29
Let’s be real-this whole thing is a distraction. Fluoroquinolones have been around for decades. If they were this dangerous, we’d have seen mass outbreaks. The real issue? The medical system is broken. We’re overmedicating everyone. But blaming one class of antibiotics? That’s just scapegoating. The problem isn’t cipro-it’s that we treat every sniffle like a crisis.
Chris porto January 4, 2026 AT 02:39
That’s the thing. The system doesn’t care until someone’s grandmother ends up in a nursing home. Then suddenly it’s a tragedy. But if you stop it early? They go home. It’s not about avoiding antibiotics. It’s about choosing the right one. And that’s not hard. It’s just not taught.
Write a comment