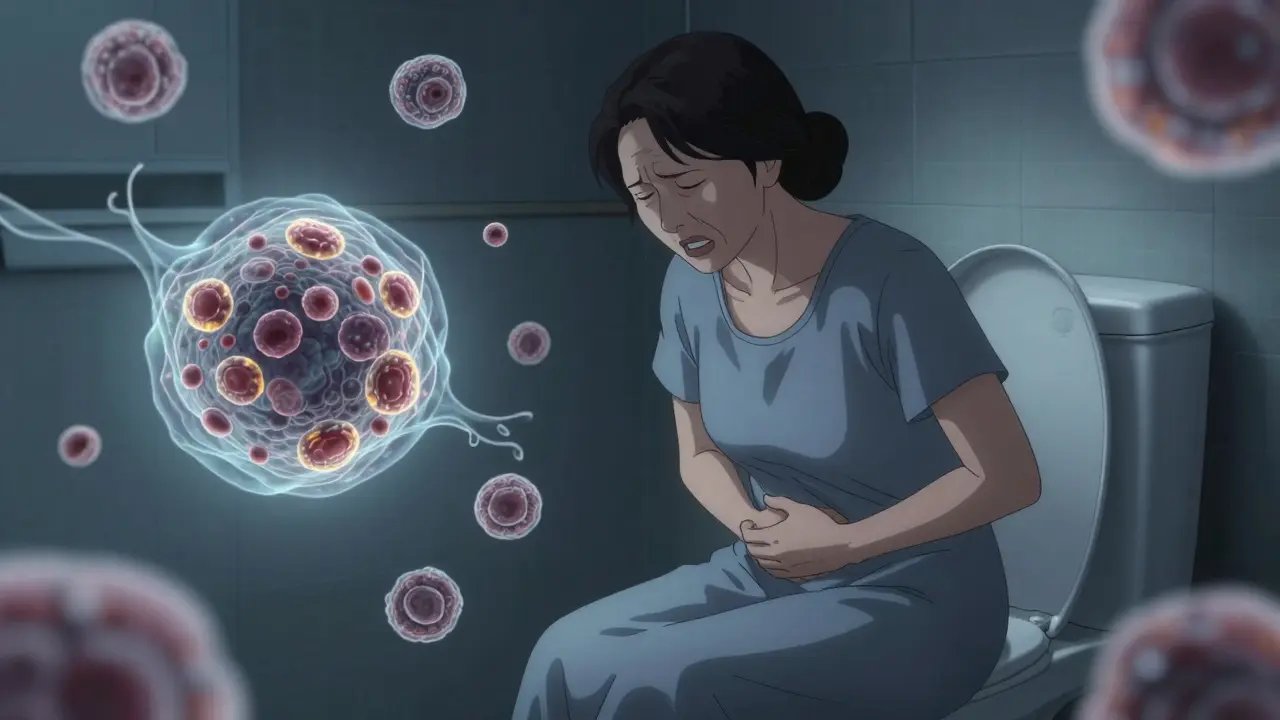
Chronic diarrhea that won’t go away-no blood, no fever, no obvious cause-can be one of the most frustrating health problems to live with. If you’ve been dealing with 5 to 10 watery bowel movements a day for months, and colonoscopies keep coming back "normal," you might have microscopic colitis. It’s not as well-known as Crohn’s or ulcerative colitis, but it’s just as real. And for most people, the answer lies in a single drug: budesonide.
What Is Microscopic Colitis?
Microscopic colitis isn’t one disease. It’s two: collagenous colitis and lymphocytic colitis. Both cause the same symptoms: persistent, watery diarrhea without blood. You might also have abdominal cramps, weight loss, or need to wake up at night to use the bathroom. The big twist? Your colon looks perfectly normal during a colonoscopy. That’s why it’s called microscopic-you need a biopsy, looked at under a microscope, to see the problem. In lymphocytic colitis, there’s an overload of white blood cells inside the colon lining. In collagenous colitis, a thick band of collagen-like scar tissue-builds up under the lining. Either way, the colon can’t absorb water properly. That’s why the stool is always liquid. It mostly affects people over 60, and women are twice as likely to get it as men. The average time from first symptoms to diagnosis? About 11 months. Many people are told they have IBS, take antidiarrheals, and wait-sometimes for years-before someone orders the right biopsy.Why Budesonide Is the First-Line Treatment
Before budesonide, doctors used prednisone, a strong steroid. It worked-but it came with a price: weight gain, high blood sugar, mood swings, and bone thinning. For older adults, that’s a dangerous trade-off. Budesonide changed everything. It’s a steroid, yes-but it’s designed to work mostly in the gut. About 90% of it gets broken down by the liver before it enters your bloodstream. That means less damage to your bones, blood sugar, or adrenal glands. In clinical trials, 75% to 85% of people with microscopic colitis go into remission after 6 to 8 weeks of taking 9 mg daily. Compare that to placebo, where only 25% feel better. One major study showed that 84% of collagenous colitis patients had complete symptom relief with budesonide, versus just 38% on sugar pills. The results were so clear, guidelines across Europe and North America now say: start with budesonide. It’s not just effective-it’s the safest steroid option for this condition.How It Works and What to Expect
You’ll take one 9 mg capsule daily, usually in the morning. Most people notice improvement within 10 to 14 days. Some go from 10 bowel movements a day to 2 or 3. That kind of change doesn’t just help physically-it restores your life. People on forums like Reddit describe it as "getting their life back." But it’s not magic. Symptoms often come back after you stop. About half of patients relapse within a year of stopping budesonide. That’s why many need a maintenance dose-usually 6 mg daily, sometimes lower. For some, that means staying on it for years. Your doctor will likely check your bone density before starting, especially if you’re over 50. They might also test your blood sugar and blood pressure. Even with its low side effect profile, budesonide isn’t risk-free. Some people report insomnia, acne, or mood changes. But compared to prednisone, these are rare and mild.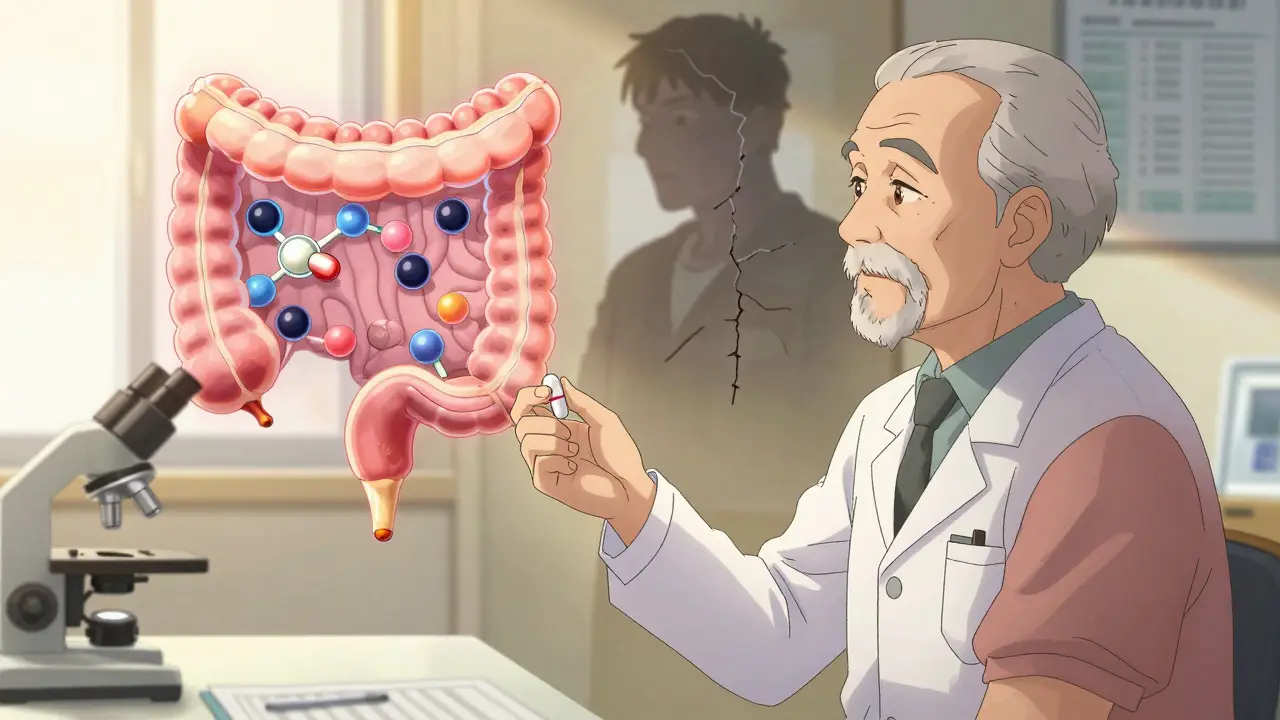
What If Budesonide Doesn’t Work?
About 15% to 20% of people don’t respond. In those cases, doctors turn to alternatives. Bismuth subsalicylate (Pepto-Bismol) helps about 26% of patients. Cholestyramine, a bile acid binder, works well if bile malabsorption is the trigger-about 60% to 70% respond. Mesalamine, used for ulcerative colitis, helps 40% to 50%. None of these come close to budesonide’s success rate. Anti-TNF drugs like infliximab? They’re expensive ($2,500 per infusion) and only help 20% to 30% of people. They’re reserved for cases where everything else fails. New drugs are coming. Vedolizumab, an antibody targeting gut inflammation, showed 65% remission in early trials and is now in fast-track review by the FDA. But it’s not available yet. For now, budesonide remains the gold standard.Cost, Access, and Real-World Challenges
The good news? Generic budesonide hit the market in 2018. A full 8-week course now costs $150 to $250-down from $800 to $1,200 for the brand-name Entocort EC. That’s made it accessible for most patients with insurance. But without insurance? Even $200 can be a barrier. And tapering off is tricky. If you stop too fast, symptoms return. Most doctors recommend cutting the dose by 3 mg every 2 to 4 weeks. Some patients need to stay on 3 mg daily long-term just to stay symptom-free. One Reddit user wrote: "Worked great for 6 weeks. Then my diarrhea came back. Now I’m on maintenance for two years. I don’t want to be on steroids forever, but I don’t want to go back to the bathroom every hour, either." That’s the reality. For many, budesonide isn’t a cure-it’s a management tool. And that’s okay.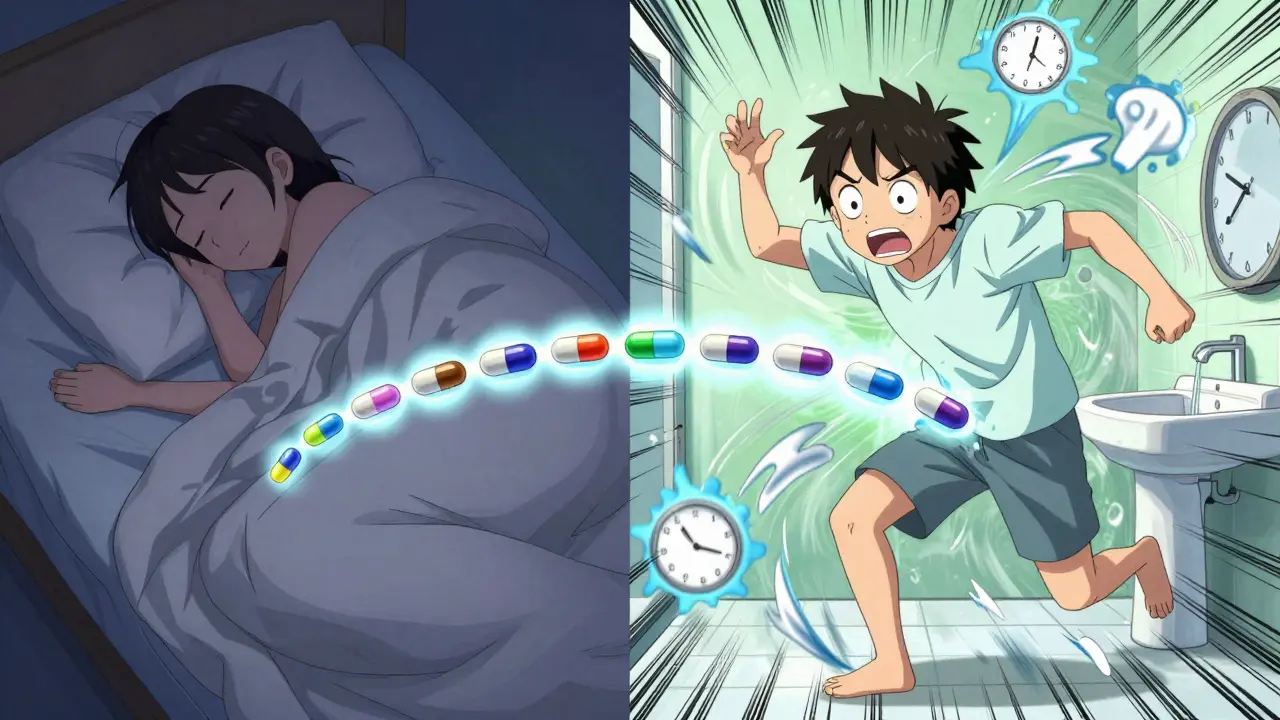






Posts Comments
Donna Peplinskie January 2, 2026 AT 16:09
I’ve been living with this for years, and I can’t tell you how relieved I was when my doctor finally ordered the biopsy. I thought I was just "anxious" or had IBS. No one took me seriously until they looked under the microscope. Budesonide didn’t fix everything, but it gave me back my weekends, my sleep, and my dignity. Thank you for writing this - it’s the kind of post I wish I’d found five years ago.
Also, if anyone’s struggling with the cost - ask about patient assistance programs. I got mine for $5 a month through the manufacturer. You’re not alone.
Alex Warden January 2, 2026 AT 18:27
This is why America needs better doctors. Back in my day, you didn’t need a fancy biopsy - you just took Pepto and stopped whining. Now everyone’s on steroids for diarrhea like it’s a vitamin. What’s next, a pill for sneezing?
Todd Nickel January 4, 2026 AT 12:38
It’s fascinating how budesonide’s first-pass metabolism in the liver reduces systemic exposure while maintaining local efficacy in the colon. The pharmacokinetic profile is elegantly engineered - 90% hepatic extraction means minimal adrenal suppression compared to prednisone, which has near-complete bioavailability. This isn’t just a drug; it’s a targeted delivery system disguised as a capsule. The clinical data is robust: RCTs consistently show remission rates 3x higher than placebo, with a number needed to treat (NNT) of approximately 1.8. What’s underdiscussed is the long-term mucosal healing potential - most studies only track symptom relief, not histological normalization. I’d love to see longitudinal biopsy data over 5+ years.
Also, the HLA-DQ2/8 association is compelling. If validated, it could shift this from a symptom-based diagnosis to a precision medicine paradigm. The COLMICS trial is a step in the right direction, but sample sizes are still small. More data needed.
Austin Mac-Anabraba January 5, 2026 AT 13:09
Of course it works - it’s a steroid. The real question is why we’re still treating symptoms instead of asking why this is happening in the first place. Who’s getting sick? Why now? Why women? Why over 60? There’s a pattern here, and it’s not just bad luck. It’s the food, the water, the chemicals in everything. They’ve been poisoning us for decades and now they want to sell us a $200 pill to make us feel better while the system keeps dumping toxins into our soil and air. Budesonide doesn’t fix the problem - it just lets you ignore it longer.
And don’t get me started on the pharmaceutical lobby pushing this as a "gold standard." They’ve been doing this since the 70s. Profit over people. Always.
Phoebe McKenzie January 7, 2026 AT 06:07
THIS IS WHY WE CAN’T HAVE NICE THINGS. You people are so desperate for a quick fix that you’re willing to swallow a steroid like it’s candy. Do you even know what steroids do to your body long-term? Bone loss? Mood swings? Diabetes? You’re trading one hell for another. And now you’re praising it like it’s a miracle? This isn’t medicine - it’s chemical surrender. If you’d just cut out gluten, dairy, and processed sugar - which, by the way, are in EVERYTHING - you wouldn’t need this crap. But no, you’d rather take a pill and call it a day. Pathetic.
gerard najera January 9, 2026 AT 00:32
Budesonide works. But it’s not a cure. Accept that.
Stephen Gikuma January 10, 2026 AT 10:02
Did you know budesonide was developed by a company linked to the CDC? And that the FDA fast-tracked it right after the 2018 patent expiration? Coincidence? I don’t think so. They want you dependent on it. Why? Because if you’re taking budesonide, you’re not asking questions about the water supply, the vaccines, or the glyphosate in your bread. They don’t want you to know the truth - they want you medicated and quiet.
And now they’re pushing genetic testing to make you feel like it’s your fault you got sick. Wake up.
Bobby Collins January 11, 2026 AT 03:52
Wait so like… is this just like… gluten? I tried going gluten-free and my diarrhea got better for a bit but then came back. So I dunno. I think it’s the water. Or the 5G. Or both. My cousin’s friend’s dog had the same thing after the wifi tower went up. Just saying.
Also, budesonide? Sounds like a brand of energy drink. 😅
Layla Anna January 12, 2026 AT 11:09
I’m so glad someone finally wrote this in a way that doesn’t make you feel crazy. I cried when I read the part about "getting your life back" - that’s exactly what it felt like. I used to avoid parties because I didn’t know where the bathroom was. Now I travel. I hug people. I sleep through the night.
Also, if you’re on budesonide and you’re scared to taper - you’re not alone. I’ve been on 3mg for 3 years. My doctor says it’s fine. I say I’d rather be safe than sorry. You’re not weak for needing it. You’re brave for staying alive.
❤️
Heather Josey January 13, 2026 AT 09:30
Thank you for this comprehensive, compassionate, and clinically accurate overview. As a healthcare provider, I’ve seen too many patients suffer for years due to diagnostic delays. This post could save lives. I’ve already shared it with my GI colleagues and patients. The emphasis on biopsy over colonoscopy alone is critical - too many are missed because the colon "looks normal."
Also, the cost reduction since generic availability is a major win. We must continue advocating for affordable access, especially for uninsured patients. And yes - maintenance dosing is not failure. It’s smart medicine.
Well done.
Write a comment