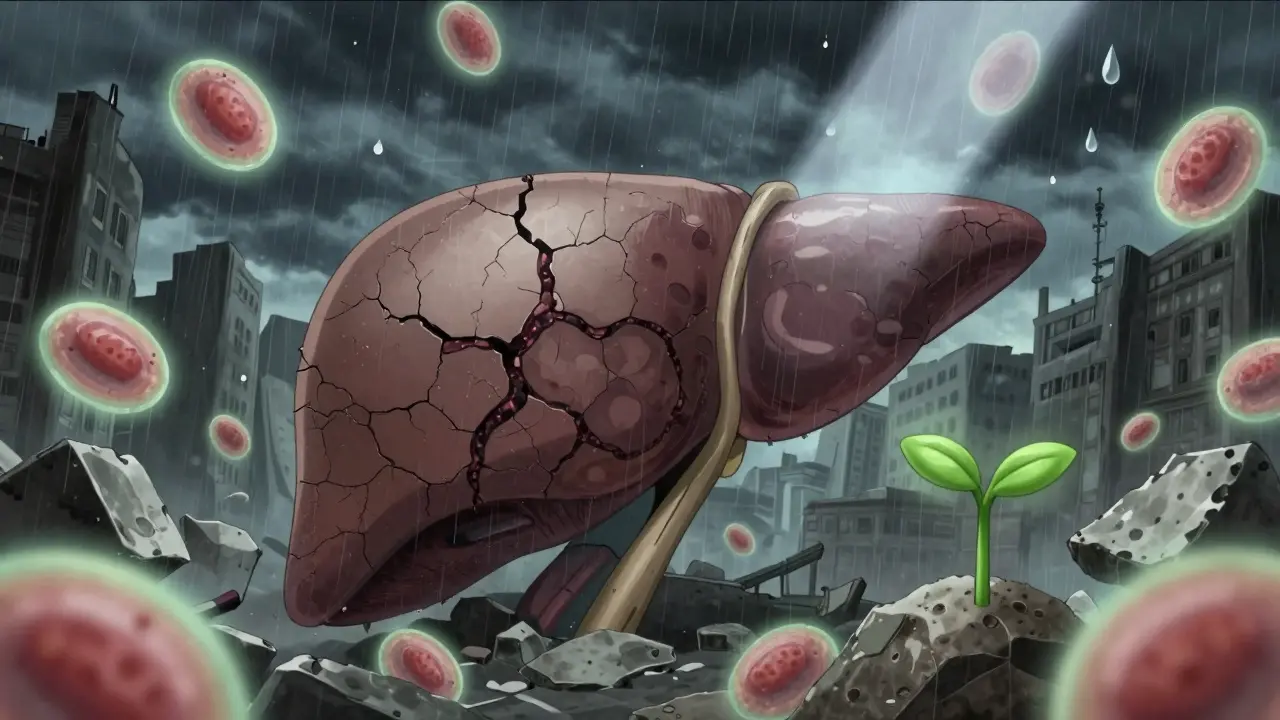
When your liver starts to scar, it’s not just a minor glitch-it’s a slow-motion crisis. Cirrhosis isn’t a single disease. It’s the end result of years of damage, where healthy liver tissue gets replaced by stiff, useless scar tissue. By the time most people are diagnosed, the liver has already lost much of its ability to function. And once that scarring becomes severe, it’s permanent. No pill can undo it. But understanding what’s happening inside your body can make all the difference between managing the condition and facing life-threatening complications.
What Exactly Is Cirrhosis?
Cirrhosis means your liver is covered in scars. Not just a few, but enough to change its entire structure. Think of it like a sponge that’s been dried out and hardened over time. Instead of soft, flexible tissue that filters toxins, produces proteins, and stores energy, you now have thick bands of fibrous tissue wrapping around small islands of surviving liver cells. These scars block blood flow, mess up chemical processing, and stop the liver from doing its job. The term comes from the Greek word kirrhos, meaning tawny yellow-the color a damaged liver turns. This isn’t just a description; it’s a warning sign. The liver is one of the few organs that can regenerate. But when damage keeps coming-whether from alcohol, hepatitis, or fatty liver disease-it can’t keep up. Scar tissue piles up faster than new cells can replace them. There are two stages: compensated and decompensated. In compensated cirrhosis, your liver is scarred but still managing to keep you alive. You might feel fine, or just tired. Blood tests might show abnormalities, but no major symptoms yet. That’s the window to act. Once you hit decompensated cirrhosis, things go downhill fast. Fluid builds up in your belly (ascites), your brain gets foggy (hepatic encephalopathy), you start bleeding easily, and your kidneys struggle. Survival rates drop sharply here-from 80-90% over five years in compensated cases to just 20-50% in decompensated ones.How Do You Know If You Have It?
Many people don’t know they have cirrhosis until it’s advanced. That’s because early on, there are no obvious symptoms. Routine blood work might show elevated liver enzymes, or a low platelet count, and that’s often the first clue. A patient in their 50s, never told they had hepatitis C, finds out their liver is already scarred after a simple checkup. That’s not rare. Doctors use a mix of tools to confirm cirrhosis. Blood tests check for high bilirubin, low albumin, and prolonged clotting time. A platelet count below 150,000 is another red flag-often caused by an enlarged spleen from increased pressure in the liver’s blood vessels. Imaging like ultrasound elastography measures liver stiffness. If it’s above 12.5 kPa, cirrhosis is likely. MRI elastography is even more accurate, hitting 90% precision. Liver biopsy used to be the gold standard. Now, non-invasive tests are replacing it in most cases. But they’re not perfect. Inflammation from a recent infection or heart failure can make the liver appear stiffer than it really is. That’s why doctors don’t rely on one test alone. They look at your history, symptoms, labs, and scans together.What Causes It?
Cirrhosis doesn’t appear out of nowhere. It’s the result of long-term damage. The biggest causes in the U.S. today are:- Non-alcoholic fatty liver disease (NAFLD) - now the top cause, affecting 24% of cirrhosis patients. Often tied to obesity, diabetes, or high cholesterol.
- Alcohol-related liver disease - still a major player, especially in people who drink heavily over many years.
- Hepatitis B and C - chronic viral infections that silently damage the liver for decades. Hepatitis C, in particular, can go undetected for years.
- Autoimmune hepatitis - the body’s immune system attacks the liver.
- Primary biliary cholangitis - a rare condition where bile ducts slowly get destroyed.
What Happens When the Liver Fails?
When cirrhosis progresses to failure, your body starts breaking down in ways you can’t ignore.- Ascites - fluid pools in your abdomen, making you bloated, uncomfortable, and at risk for infection. Removing it helps, but you need albumin infusions to keep your blood pressure stable.
- Hepatic encephalopathy - toxins your liver can’t filter build up in your brain. You might forget things, get confused, slur your speech, or even fall into a coma. It’s treatable, but it often comes back.
- Bleeding - scar tissue raises pressure in the portal vein, causing swollen veins in your esophagus or stomach. These can rupture suddenly and cause life-threatening bleeding.
- Kidney problems - the liver and kidneys work together. When the liver fails, the kidneys often follow.
Liver Transplant: The Only Real Cure
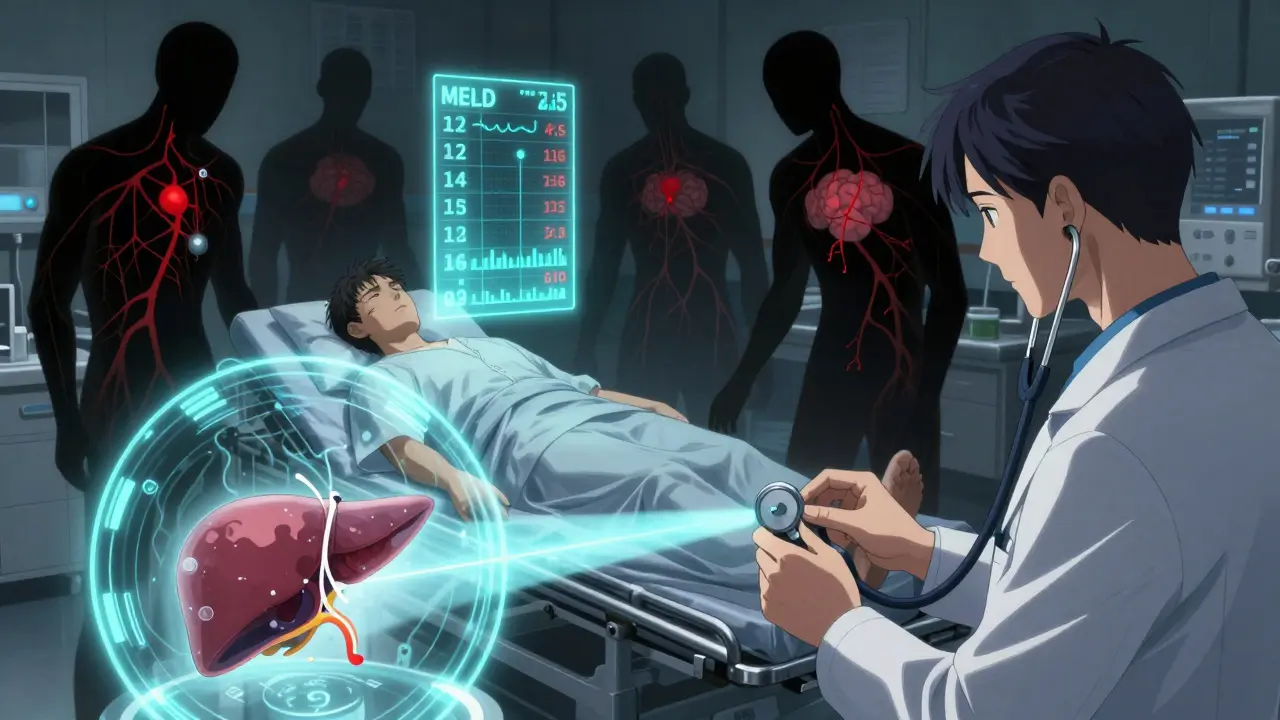
There’s no drug that can reverse cirrhosis. No supplement, no diet, no miracle treatment. The only thing that can truly replace a failed liver is a transplant. In the U.S., cirrhosis is the leading reason for liver transplants-about 40% of all cases. But here’s the hard truth: there aren’t enough organs. In 2022, 8,780 transplants were done. Over 14,300 people were on the waiting list. That means about 12% of people on the list die each year before they get a liver. The system prioritizes who gets a liver based on MELD-Na scores, which also factor in sodium levels. The sicker you are, the higher your priority. But that doesn’t mean you’re guaranteed a transplant. You have to be healthy enough to survive the surgery. That means quitting alcohol, losing weight if needed, and getting your infections under control. New tech is helping. Machines that keep donor livers alive and beating outside the body (normothermic perfusion) have increased the number of usable organs by 22%. Researchers are also testing bioartificial livers and stem cell therapies. Early trials show promise-some patients saw MELD scores drop by 40% after cell treatments. But these are still experimental.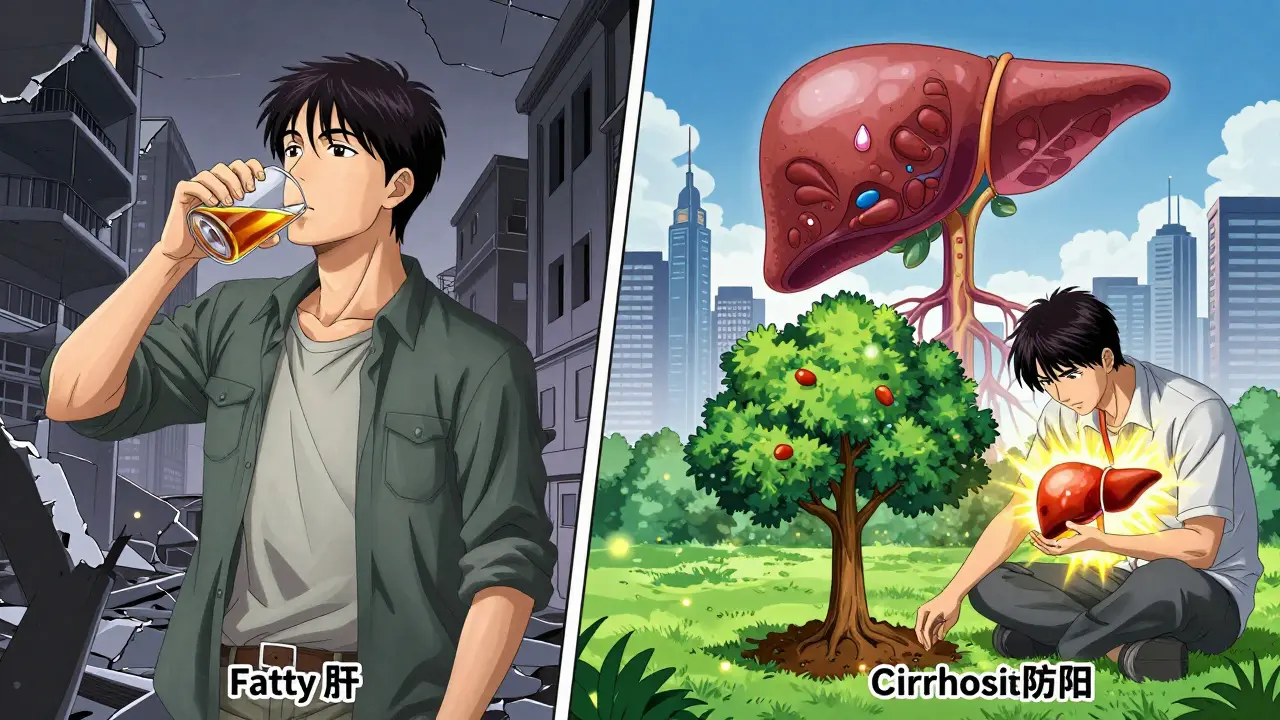
Can You Manage It Without a Transplant?
Yes-sometimes. But only if you’re caught early and you stick to the plan.- Stop drinking - if alcohol is the cause, quitting is non-negotiable. Even small amounts can push you into decompensation.
- Lower sodium - less than 2,000 mg a day. That means no canned food, no processed snacks, no soy sauce. It’s hard, but it reduces fluid buildup.
- Treat the cause - antivirals for hepatitis, weight loss and diabetes control for fatty liver, immunosuppressants for autoimmune disease.
- Take prescribed meds - lactulose for brain fog, beta-blockers to prevent bleeding, diuretics to drain fluid.
- Get monitored - regular ultrasounds to check for liver cancer, blood tests every few months.
What’s Next for Cirrhosis Treatment?
The future is shifting from treating symptoms to stopping the scarring itself. In 2023, a phase 3 trial showed a drug called simtuzumab slowed fibrosis progression in NASH-related cirrhosis by 30%. That’s not a cure, but it’s progress. Experts believe that within five years, treatment will be personalized. Instead of just using MELD scores, doctors might look at your liver’s molecular signature-how your genes and proteins are reacting to damage. That could mean targeted drugs for specific types of scarring. But the biggest challenge remains: organ shortage. Even with better tech, we can’t grow livers yet. Until we can, the best defense is early detection and stopping damage before it starts.What Should You Do If You’re Diagnosed?
If you’ve been told you have cirrhosis, don’t panic-but don’t delay either. Here’s what to do next:- Find a hepatologist-a liver specialist. General doctors don’t have the depth of experience needed.
- Get a full workup: blood tests, imaging, and a MELD score calculation.
- Identify and treat the root cause. This is your most powerful tool.
- Join a support program. The American Liver Foundation offers nurse navigation (1-800-GO-LIVER) and connects you with local resources.
- Start making lifestyle changes now-even if you feel fine. Your liver doesn’t have time to wait.
Can cirrhosis be reversed?
Early liver scarring (fibrosis) can sometimes be reversed if the cause is removed-like stopping alcohol or curing hepatitis C. But once cirrhosis is established, the scar tissue is permanent. No medication can undo it. The focus shifts to preventing further damage and managing complications.
What’s the difference between fatty liver and cirrhosis?
Fatty liver means excess fat builds up in liver cells-it’s often reversible with weight loss and better diet. Cirrhosis is when that fat, or other damage, leads to permanent scarring and structural changes. Fatty liver can turn into cirrhosis if left unchecked, but not everyone with fatty liver gets cirrhosis.
How long can you live with cirrhosis?
It depends on the stage. With compensated cirrhosis and good management, many live 10-15 years or more. Once decompensated, survival drops to 2-5 years without a transplant. MELD scores help predict this-higher scores mean shorter life expectancy.
Is a liver transplant the only option for advanced cirrhosis?
For end-stage cirrhosis, yes. No drug can replace a failed liver. Transplant is the only cure. Other treatments manage symptoms but don’t fix the underlying damage. New therapies like stem cells are promising but still experimental and not widely available.
Can you drink alcohol with cirrhosis?
Absolutely not. Even small amounts of alcohol can cause rapid worsening of liver damage and push you into liver failure. If alcohol caused your cirrhosis, quitting is the single most important step you can take. If it didn’t, alcohol still adds stress to a damaged organ-so avoid it completely.





Posts Comments
LOUIS YOUANES January 29, 2026 AT 22:49
This post reads like a pharmaceutical ad disguised as medical advice. They didn’t mention the real culprit: corporate greed and insurance loopholes that keep people from getting tested until it’s too late.
Laia Freeman January 30, 2026 AT 14:06
OMG I JUST FOUND OUT I HAVE FATTY LIVER AND I’M LIKE 32???!?!?!? I’M GONNA DIE RIGHT??!!??!!??
Laura Arnal January 31, 2026 AT 06:48
You got this!! 💪 Fatty liver is totally reversible if you start now-cut the sugar, walk 30 mins a day, and drink water instead of soda. You’re not alone!! 🌱❤️
Write a comment