For millions of people, a glass of milk, a scoop of ice cream, or even a slice of cheese can trigger bloating, cramps, gas, or diarrhea. It’s not an allergy. It’s not just being "sensitive." It’s lactose intolerance - a common, often misunderstood condition where the body can’t properly digest lactose, the natural sugar in milk. The good news? You don’t have to give up all dairy. The better news? There’s a clear path to knowing for sure if it’s lactose - and how to manage it without feeling sick or missing out.
What Exactly Is Lactose Intolerance?
Lactose intolerance happens when your small intestine doesn’t make enough of an enzyme called lactase. Lactase breaks down lactose into simpler sugars your body can absorb. Without it, lactose moves undigested into your colon, where bacteria ferment it. That fermentation is what causes the gas, bloating, cramps, and diarrhea. It’s not an immune reaction like a milk allergy - it’s purely a digestive issue.
This isn’t something you’re born with in most cases. Almost all babies produce lactase - that’s how they digest breast milk. But after weaning, many people naturally reduce lactase production. This is called lactase non-persistence, and it’s the most common form. By adulthood, about 68% of the global population has some level of lactase deficiency, with rates above 90% in East Asian populations and below 10% in Northern Europeans.
What’s confusing is that not everyone with low lactase has symptoms. Some people can drink a glass of milk with no problem. Others get sick from a tablespoon of cream. That’s why diagnosis isn’t just about lab tests - it’s about your body’s real-world response.
How Do You Know If It’s Lactose Intolerance?
Doctors don’t just hand out diagnoses based on symptoms. Too many other conditions - like IBS, celiac disease, or even food sensitivities - can mimic lactose intolerance. The first step is always ruling out other causes. But if your symptoms line up with dairy intake, here’s how it’s confirmed.
The most reliable test is the hydrogen breath test. You drink a liquid with 25-50 grams of lactose (roughly 1-2 cups of milk). Then, every 30 minutes for 2-3 hours, you blow into a device that measures hydrogen in your breath. If your body can’t digest the lactose, gut bacteria ferment it and release hydrogen. A spike of more than 20 parts per million above your baseline means you’re malabsorbing lactose. This test is 90% accurate and non-invasive.
There’s also a blood test - you drink lactose and get your blood sugar checked every 30 minutes. If your glucose doesn’t rise by at least 20 mg/dL, your body isn’t breaking down the sugar. But this test is outdated. It’s less accurate, requires multiple needle sticks, and can give false results because of how fast your stomach empties.
For kids under 5, doctors use a stool acidity test. Undigested lactose turns into acids in the colon, making stool more acidic. A pH below 5.5 is a red flag.
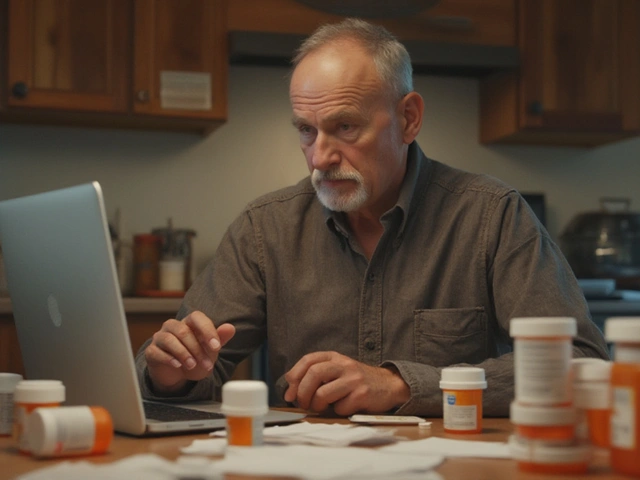
But here’s the truth most people don’t hear: you don’t always need a test. Many doctors, especially in primary care, recommend starting with a simple elimination diet. Cut out all dairy for 2-4 weeks. If your symptoms vanish, then slowly add back small amounts of milk, yogurt, or cheese. If symptoms return, it’s likely lactose. This method is low-cost, personal, and reflects how your body actually reacts - not just what a machine says.
Why the Hydrogen Breath Test Isn’t Perfect
Even the best test has flaws. The hydrogen breath test can give false positives if you have small intestinal bacterial overgrowth (SIBO), which affects about 15% of people. Antibiotics, recent stomach infections, or even certain diets can throw off results. That’s why guidelines now say: don’t test unless you’re planning to change your diet. And never rely on the test alone.
Dr. E. M. Weaver, a leading researcher, puts it plainly: “A positive test without symptoms isn’t lactose intolerance. It’s just malabsorption.” Many people test positive but never have symptoms. Others test negative but still feel awful after dairy. That’s why the American Gastroenterological Association says diagnosis should be based on symptom response - not test results.
Another problem? Overdiagnosis. A 2023 study in JAMA Internal Medicine found that 35% of people diagnosed with lactose intolerance via breath test could actually tolerate normal dairy portions without issues. That means thousands of people are avoiding dairy unnecessarily - risking bone health and missing out on nutrients.

How Much Lactose Can You Actually Tolerate?
The biggest myth? That you have to cut out all dairy forever. That’s not true for most people.
Research shows the average adult can handle up to 12 grams of lactose in one sitting - that’s about one cup of milk. Many people can even handle 18 grams if they eat it with food. Hard cheeses like cheddar or parmesan have almost no lactose - it’s mostly drained off during aging. Yogurt, especially Greek yogurt, is often well-tolerated because the live cultures help break down lactose.
Here’s a simple guide to common foods:
- 1 cup milk (240 ml): 12g lactose
- 1 cup yogurt: 9-12g lactose
- 1 oz hard cheese (cheddar, parmesan): 0.1-0.5g lactose
- 1/2 cup ice cream: 6g lactose
- 1 slice of bread: 0-2g lactose (hidden in some brands)
You don’t need to be perfect. Start small. Try a quarter cup of milk with breakfast. Wait a few hours. See how you feel. Track it. You might be surprised.
Dietary Management: What to Eat and What to Avoid
If you’re cutting back on dairy, you need to replace the nutrients - especially calcium and vitamin D. The average adult needs 1,000-1,200 mg of calcium daily. Dairy is the easiest source, but it’s not the only one.
Good non-dairy calcium sources:
- Fortified plant milks (soy, oat, almond): 300-500 mg per 8 oz
- Fortified orange juice: 300 mg per cup
- Calcium-set tofu: 200-400 mg per 1/2 cup
- Collard greens, kale, bok choy: 100-250 mg per cooked cup
- Canned sardines or salmon with bones: 300 mg per 3 oz
Vitamin D is trickier. Few foods have it naturally. Sun exposure helps, but many people need supplements. Look for 600-800 IU daily if you’re not getting sunlight.
Watch out for hidden lactose. It’s in processed foods you wouldn’t expect: bread, cereal, salad dressings, protein bars, and even some medications. The FDA now requires products labeled “lactose-free” to contain less than 0.01% lactose - but “dairy-free” doesn’t mean the same thing. Always check the ingredient list for milk solids, whey, casein, or milk sugar.
Supplements and New Options
Lactase enzyme pills - like Lactaid® - are a game-changer. Take 3,000-9,000 FCC units right before eating dairy. Studies show they reduce symptoms by 70-90%. They’re not magic, but they give you freedom. You can have pizza, ice cream, or mac and cheese without fear.
Newer options are emerging. Pendulum Therapeutics’ LactoSpore® probiotic, tested in 2023, helped participants digest 40% more lactose than placebo. It’s not yet widely available, but it points to a future where gut bacteria help you digest what you eat.
There’s also a new rapid breath test called LactoQuik®, approved in 2022. It gives results in 45 minutes instead of 3 hours. Faster, cheaper, and just as accurate. It’s starting to show up in larger clinics.
What About Kids and Teens?
Parents often panic when a child complains of stomach pain after milk. But cutting out dairy too early can harm growth. The European Food Safety Authority recommends lactose tolerance thresholds by age:
- Adults: up to 12g per sitting
- Children 4-8: up to 8g
- Children under 4: up to 4g
For young kids, yogurt and hard cheese are safer than milk. If you’re unsure, talk to a pediatrician. Don’t assume every belly ache is lactose. Many kids outgrow mild intolerance. And never cut out dairy without checking calcium and vitamin D levels.
Real Stories, Real Challenges
On Reddit, one user waited eight months for a breath test in the UK NHS - diagnosed with IBS in the meantime. Another, after eliminating dairy for three weeks, saw her chronic diarrhea vanish. “The test just confirmed what my body already told me,” she said.
But 58% of patients in a Cleveland Clinic survey struggled to get enough calcium after diagnosis. Many felt isolated at restaurants or family dinners. The biggest complaint? “One-size-fits-all” advice. You’re told to avoid all dairy - but then you find out you can eat yogurt, cheese, and even a splash of milk in coffee.
Personalization is the future. Apps like MyLactaseTracker® let you log what you eat and how you feel. Over time, you build your own tolerance map. No two people are the same.
Final Takeaway: It’s Not All or Nothing
Lactose intolerance isn’t a life sentence. It’s a signal - your body telling you how much it can handle. You don’t need to become a label-reader forever. You don’t need to give up cheese. You don’t need to buy expensive alternatives unless you want to.
Start with the elimination diet. Track your symptoms. Reintroduce slowly. Use enzyme pills when you want to enjoy something special. Choose calcium-rich foods you like. And if you’re unsure - get tested, but don’t let the test decide your life.
You can still eat well. You can still feel good. You just need to find your own balance - not someone else’s rules.
Can lactose intolerance develop later in life?
Yes. Lactase production naturally declines after childhood in most people. This is called lactase non-persistence and is the most common cause of lactose intolerance in adults. It can also develop after illness, surgery, or injury to the small intestine - this is called secondary lactose intolerance and may be temporary.
Is lactose intolerance the same as a milk allergy?
No. A milk allergy is an immune system reaction to milk proteins like casein or whey. It can cause hives, swelling, vomiting, or even anaphylaxis. Lactose intolerance is a digestive issue caused by lack of the lactase enzyme. It causes bloating, gas, and diarrhea - not life-threatening reactions.
Do I need to avoid all dairy if I’m lactose intolerant?
No. Most people can tolerate small amounts of lactose - especially in hard cheeses, yogurt, or when eaten with meals. Many can handle up to 12 grams of lactose (about one cup of milk) without symptoms. You don’t need to cut out all dairy unless you have severe reactions.
Are lactose-free products healthier?
Not necessarily. Lactose-free milk is just regular milk with added lactase enzyme - it’s nutritionally identical. Many plant-based alternatives are fortified with calcium and vitamin D, but some are high in sugar or additives. Always check the label. Lactose-free doesn’t mean low-calorie or healthier - just dairy-free.
Can I take lactase supplements every day?
Yes. Lactase enzyme supplements like Lactaid® are safe for daily use. They’re not absorbed by the body - they just help break down lactose in your gut. Take them right before eating dairy. There’s no evidence of long-term side effects or dependency.
Why do some people with lactose intolerance feel fine with yogurt but not milk?
Yogurt contains live cultures (probiotics) that help break down lactose before you even eat it. The fermentation process reduces lactose content by up to 30%. Greek yogurt has even less because it’s strained. So even if you’re lactose intolerant, you may tolerate yogurt better than milk.
Can lactose intolerance be cured?
Primary lactose intolerance - the kind caused by genetics - can’t be cured. But secondary lactose intolerance, caused by illness or injury, may improve once the gut heals. For most people, management through diet, supplements, and gradual exposure is the best long-term strategy.





Posts Comments
Shante Ajadeen November 13, 2025 AT 01:33
OMG I literally just figured this out last year. Thought I was just "sensitive" to dairy until I cut it out for a month and my bloating vanished. Now I just take a Lactaid before pizza and life’s good. No need to be scared of cheese anymore.
Also, yogurt is my best friend. Greek yogurt with berries? Perfect. Milk? Nope. But I didn’t need a test to know that.
dace yates November 13, 2025 AT 19:29
I’ve been avoiding dairy for years because I assumed I was intolerant, but I never got tested. I just felt weird after milk. But then I tried a tiny bit of cheddar on my burger last week and felt zero issues. Now I’m wondering if I ever really had it at all.
Maybe the real issue is we’re all overthinking this.
Danae Miley November 14, 2025 AT 11:26
There’s a critical flaw in the article’s implication that the hydrogen breath test is reliable. It doesn’t account for SIBO, which is vastly underdiagnosed. A positive result doesn’t equal lactose intolerance-it equals bacterial fermentation. Many patients are misdiagnosed and put on unnecessary diets while their real gut issue goes untreated.
The American Gastroenterological Association’s stance is correct: symptoms + response to challenge, not test results, define diagnosis. Relying on breath tests alone is medical negligence in primary care settings.
Charles Lewis November 15, 2025 AT 17:35
It is imperative to recognize that lactose intolerance, while common, is not a monolithic condition, nor is it universally applicable in its management. The physiological variance among individuals, particularly in terms of colonic microbiota composition, gastric emptying rates, and dietary context, renders blanket recommendations-such as the 12-gram threshold-potentially misleading.
Moreover, the nutritional implications of dairy avoidance cannot be overstated. Calcium and vitamin D are not interchangeable through fortification alone; bioavailability varies significantly across plant-based sources. For instance, oxalates in spinach inhibit calcium absorption, rendering it functionally inferior to dairy or fortified soy milk.
Therefore, a personalized, longitudinal approach, ideally under the guidance of a registered dietitian, is not merely advisable-it is medically necessary. The proliferation of anecdotal advice online has led to a public health dilemma: unnecessary dietary restriction without nutritional oversight.
Renee Ruth November 16, 2025 AT 18:50
Okay but have you considered that maybe your entire life has been a lie?
I mean, I got diagnosed with lactose intolerance at 22, cut out dairy, felt amazing… then I accidentally had a slice of pizza at a party and cried because I felt SO GOOD. Like, my skin cleared up, my energy was insane. Turns out I had SIBO the whole time and the lactose was just a symptom.
Now I’m on antibiotics and I can eat ice cream again. But nobody warned me. The system failed me. And now I’m mad.
Samantha Wade November 18, 2025 AT 16:58
This article is excellent-clear, evidence-based, and compassionate. But I want to emphasize one thing: if you’re cutting out dairy, you MUST replace the nutrients. Calcium isn’t optional. Vitamin D isn’t a suggestion.
I’ve seen too many young women with osteopenia because they went dairy-free without planning. Don’t just swap milk for almond milk and call it a day. Check the label-many are loaded with sugar and lack adequate calcium. Opt for fortified soy milk (it’s closest to dairy nutritionally), canned fish with bones, leafy greens, and consider a supplement if your intake is low.
You don’t have to suffer. You just have to be informed. And if you’re unsure? Talk to a dietitian. It’s worth the investment.
Elizabeth Buján November 20, 2025 AT 06:15
so i tried the elimination thing and honestly? i thought i was gonna miss cheese so bad… but then i realized i didn’t even crave it. like, at all.
and then i found this vegan cheddar that tastes like a memory of cheese? and now i eat it on toast and cry a little because life is weird.
also i took lactase pills once and felt like a wizard. like, i ate ice cream and didn’t turn into a gassy ghost. magic.
you’re not broken. you’re just… differently wired. and that’s cool.
Andrew Forthmuller November 22, 2025 AT 00:43
lactase pills work. try them before pizza. no test needed.
Write a comment