Palliative Care Medication Trade-off Calculator
Choose a Symptom to Explore
Management Options
Medications and their effectiveness versus side effect profile
When someone is living with a serious illness, the goal shifts from curing to comfort. That’s the heart of palliative and hospice care. It’s not about giving up. It’s about making sure every day feels as good as it can - even when time is short. But here’s the real challenge: the medicines that ease pain, breathlessness, or nausea often bring their own problems. Too much sedation. Dry mouth. Confusion. Constipation that won’t quit. Balancing relief with side effects isn’t just a medical decision - it’s a deeply personal one.
What’s the Difference Between Palliative and Hospice Care?
Palliative care is for anyone with a serious illness - whether they’re still fighting cancer, living with heart failure, or managing advanced dementia. It can start at diagnosis and run alongside treatments like chemotherapy or surgery. The goal? Reduce suffering. Improve quality of life. Help patients and families make sense of tough choices.
Hospice care is a kind of palliative care - but with a specific focus. It’s for people with a life expectancy of six months or less who have decided to stop curative treatment. It’s not about giving up hope. It’s about shifting hope from cure to comfort. Hospice teams - nurses, social workers, chaplains - come to you. Home, nursing home, or hospice facility. They manage symptoms, support families, and help people die with dignity, not in a hospital bed surrounded by machines.
Both use the same tools: pain meds, anti-nausea drugs, oxygen, counseling. But hospice is the final chapter. Palliative care is the steady hand that walks with you through the whole journey.
How Do Doctors Decide What Medication to Use?
There’s no one-size-fits-all. A 72-year-old with lung cancer and severe pain needs a different approach than a 65-year-old with kidney failure and constant nausea. Doctors don’t just guess. They use clear, evidence-backed protocols.
For pain, opioids like morphine or oxycodone are first-line. But dosing isn’t fixed. It’s adjusted daily. A patient might start with 5 mg every 4 hours - then need 10 mg after a few days. Why? Because pain changes. So does the body’s ability to process drugs. Kidney or liver trouble? Dose must drop. That’s why 87% of palliative specialists say general practitioners often miss this.
For breathlessness, opioids work - even if the patient doesn’t have pain. The American Academy of Family Physicians gives this a “B” level evidence rating: meaning it’s well-supported. But oxygen alone? Often doesn’t help. And giving too much oxygen to someone with COPD can make things worse.
For nausea, it’s not just one drug. It could be ondansetron, metoclopramide, or even dexamethasone - a steroid. Each has different side effects. Steroids might help with swelling in the gut, but they can cause insomnia or mood swings.
For anxiety or agitation, lorazepam (a benzodiazepine) is common. But if a patient is confused or delirious, antipsychotics like haloperidol might be used. The catch? These can cause stiff muscles, dizziness, or even heart rhythm changes. That’s why EKGs are checked - and why they’re stopped once the patient is calm.
What Are the Most Common Side Effects - and How Are They Managed?
Side effects aren’t accidents. They’re predictable. And they’re manageable - if you know what to look for.
- Constipation - Almost everyone on opioids gets this. It’s not normal. It’s not something you just live with. Laxatives are started right away - not when it’s bad. Senna, bisacodyl, or even enemas are routine. Some patients need daily stool softeners.
- Sedation - Drowsiness is common at first. But if a patient is sleeping through meals, missing family visits, or can’t speak, the dose is too high. Doctors look for why - is it the opioid? The anxiety med? A combo? They reduce one, not all.
- Delirium - Sudden confusion, hallucinations, agitation. It’s not dementia. It’s a medical emergency. Doctors use tools like CAM-ICU to check every 12 hours. They look for causes: infection, dehydration, drug buildup. Haloperidol helps - but only if it’s not overused.
- Dry mouth - Simple, but awful. Sips of water, ice chips, lip balm. Oral swabs. Sometimes saliva substitutes. No one talks about this - but it ruins comfort fast.
- Loss of appetite - Not always a problem. Forcing food can cause choking or vomiting. Small, favorite meals. Nutritional supplements if needed. But the goal isn’t weight gain - it’s comfort.
One key rule: Don’t stack drugs. Giving three anti-nausea meds at once? That’s a recipe for confusion or falls. One at a time. Watch. Adjust.
Why Do Families Often Resist Medication?
It’s heartbreaking to see. A daughter says, “I don’t want him to be sleepy.” A son says, “If he’s on pain meds, he’s giving up.”
These fears come from myths. “Morphine kills.” “If he’s sedated, he’s not aware.” “Pain means he’s suffering.”
The truth? Pain is suffering. And uncontrolled pain can make someone unable to speak, hold a hand, or say goodbye. Sedation from medication isn’t unconsciousness - it’s peace. A patient on the right dose can still smile, recognize loved ones, whisper “I love you.”
Doctors and nurses spend time explaining this. Not with charts. With stories. “Your dad was in so much pain yesterday, he couldn’t sleep. Today, he slept for an hour - and woke up asking for your voice. That’s not losing him. That’s giving him back a moment.”
The NCHPC guidelines say families have the right to have their loved one die free of pain - with dignity. That’s not just a phrase. It’s the foundation.
How Do You Know If the Care Is Working?
It’s not about how long someone lives. It’s about how they live in that time.
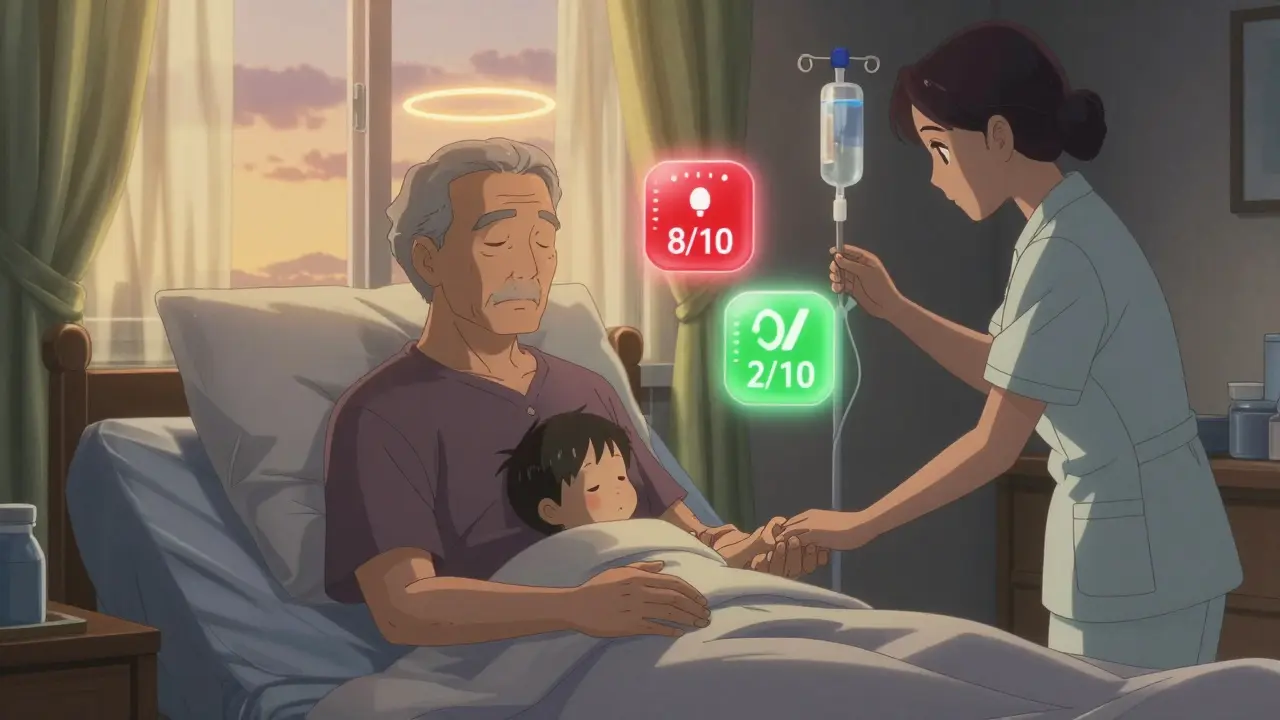
Good palliative care tracks symptoms daily. Pain on a scale of 0 to 10. Breathlessness. Nausea. Anxiety. Sleep. Mood. A patient who goes from 8/10 pain to 2/10? That’s success. A patient who can sit up, eat a spoonful of ice cream, or hold their grandchild’s hand? That’s success.
Tools like the NHS’s body diagram help patients point to where it hurts. A 31% improvement in communication? That’s huge. It means fewer mistakes. Fewer missed symptoms.
One nursing home in the UK saw a 37% jump in staff confidence after using a simple palliative care checklist. Fewer panic calls. More calm moments.
But there’s a dark side: documentation. Nurses say 68% don’t have time to fill out all the forms. That’s a problem. If you don’t write it down, you can’t adjust it. And if you don’t adjust it, side effects win.
What’s Changing in Palliative Care Right Now?
The field is evolving - fast.
Tele-palliative care is growing. In rural areas, 55% of counties have no specialist. Now, video calls let patients in remote towns get expert advice. By 2027, that could reach 40% of rural patients.
New tools are being tested. Apps that let patients report pain with one tap. Sensors that track breathing patterns. AI that flags when a patient’s symptoms are worsening before the family even notices.
And then there’s cannabis. Fraser Health added guidelines in 2023. In one study, 37% of patients needed less opioid pain meds when using cannabinoids. But 29% got dizzy. It’s not magic. It’s another tool - with risks.
The big shift? From “just treat the pain” to “treat the whole person.” That means spiritual care. Social support. Family counseling. Addressing guilt, regret, fear. Dr. Harvey Chochinov’s work shows that when people feel heard - their physical pain often drops.
And the workforce? Still short. Only 7,000 certified palliative doctors in the U.S. for 22,000 needed. That’s why every nurse, every GP, every family member needs to understand the basics.
What Should You Do If You’re Facing This?
If you or someone you love is dealing with a serious illness:
- Ask for palliative care early - even if you’re still getting treatment.
- Keep a symptom diary: pain level, sleep, appetite, mood. Bring it to appointments.
- Don’t be afraid to say, “I don’t want him to be drowsy all day.” Or “Can we try less medication?”
- Ask who’s on the team. Is there a social worker? A chaplain? A pharmacist who knows about drug interactions?
- Know that comfort isn’t weakness. It’s the most powerful thing you can give.
There’s no perfect answer. But there’s a better way - one that puts peace before prolonging, and dignity before drugs.
Is hospice care only for cancer patients?
No. Hospice care is for anyone with a life-limiting illness who has chosen comfort over cure. That includes heart failure, lung disease, kidney failure, advanced dementia, ALS, and other serious conditions. The six-month prognosis rule applies to all of them. Cancer is just the most common reason people think of hospice - but it’s far from the only one.
Can you leave hospice care if you change your mind?
Yes. Hospice is not a one-way door. If a patient’s condition improves - or if they decide to try another treatment - they can leave hospice at any time. They can re-enroll later if needed. Many patients do. It’s not a surrender. It’s a choice - and choices can change.
Do opioids shorten life?
No. When used properly, opioids don’t speed up death. In fact, uncontrolled pain can stress the body and make illness worse. Studies show that patients with well-managed pain live longer and have better quality of life. The fear that morphine “kills” comes from misunderstanding. Dosing is carefully adjusted - never rushed. The goal is comfort, not sedation.
What if my loved one refuses to take medication?
Respect their choice. Forcing medication can cause more distress than the symptom itself. Instead, ask why. Is it fear? Side effects? A belief that suffering is noble? Work with the palliative team to find alternatives - patches, suppositories, non-drug options like massage, music, or cooling fans. Sometimes, just being present is the most powerful medicine.
Are there non-drug ways to manage symptoms?
Yes - and they’re often overlooked. For breathlessness: a fan on the face, sitting upright, open windows. For pain: heat, cold packs, gentle touch, music. For anxiety: familiar voices, photos, holding hands. For nausea: ginger tea, peppermint oil, quiet rooms. These don’t replace meds - but they reduce the need for them. And that means fewer side effects.