Medication Side Effect Checker for Metallic Taste
Check if your medication causes metallic taste
Enter your medication name to see if it's associated with metallic taste side effects and get appropriate coping strategies.
Important: This tool provides general information only. Never stop taking prescribed medication without consulting your doctor. Always discuss side effects with your healthcare provider.
Nothing prepares you for the sudden taste of pennies in your mouth. You didn’t eat anything strange. You didn’t bite into a pipe. But every bite of food, every sip of water, tastes like metal. It’s not just unpleasant-it’s exhausting. You stop enjoying meals. You lose weight. You dread breakfast. If you’ve started a new medication and now everything tastes wrong, you’re not alone. About 11% of older adults on multiple drugs report this exact problem, and for people on chemotherapy or certain antibiotics, the numbers jump to over 50%.
Why Does Medication Make Your Mouth Taste Like Metal?
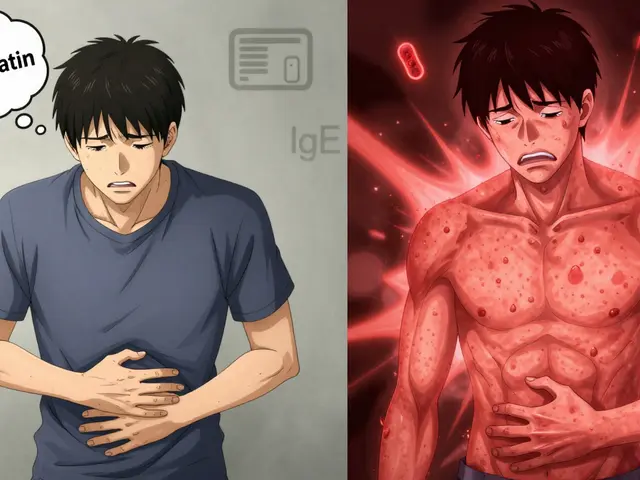
It’s not your imagination. This isn’t a minor annoyance-it’s a real physiological reaction called dysgeusia a distortion or loss of taste, often manifesting as a persistent metallic or bitter flavor without any external source. When you take a pill, your body absorbs it. Some drugs don’t just stay in your bloodstream-they show up in your saliva. That’s when the trouble starts.
Drugs like metronidazole an antibiotic commonly used for bacterial and parasitic infections, amoxicillin a penicillin-based antibiotic often prescribed for sinus and ear infections, or lithium a mood stabilizer used for bipolar disorder can directly interfere with your taste buds. Some bind to taste receptors. Others reduce zinc levels, which your taste cells need to function properly. Still others dry out your mouth by cutting saliva production-think SSRIs selective serotonin reuptake inhibitors like fluoxetine and sertraline, commonly prescribed for depression and anxiety. Without enough saliva, taste molecules can’t reach your receptors. The result? Everything tastes flat, bitter, or metallic.
Even Paxlovid an antiviral used for treating COVID-19, containing nirmatrelvir and ritonavir has this side effect. Pfizer’s own data shows nearly 58% of users report a metallic or bitter taste. It hits within hours, lasts the full five-day course, and feels like chewing aluminum foil.
How to Tell If It’s the Medication or Something Else
Not every weird taste is from a drug. Gum disease, sinus infections, or even zinc deficiency can cause similar symptoms. But here’s how to tell if your medication is the culprit:
- Did the metallic taste start within 24 to 72 hours after you began a new drug?
- Does it get worse right after you take your pill?
- Does it fade when you stop taking the medication?
If yes, it’s almost certainly drug-induced. Unlike infections, which clear up in a week or two, medication-related dysgeusia sticks around as long as you’re on the drug. And unlike dental issues, there’s usually no bleeding, swelling, or bad breath-just the taste.
One big red flag: if your doctor brushes it off as "just a side effect" and doesn’t offer solutions, you’re not getting the care you deserve. A 2022 survey found 63% of patients felt their concerns were dismissed. That needs to change.
Proven Ways to Cope With Metallic Taste
Here’s what actually works-backed by research, not just anecdote.
1. Try Zinc Supplementation
Zinc is essential for taste bud repair and function. Up to 15% of older adults are deficient, and many medications worsen this. A trial of zinc can make a dramatic difference.
- For general drug-induced dysgeusia: Take 25-50 mg of zinc gluconate daily for 2-4 weeks.
- For chemotherapy patients: 50 mg daily starting 24 hours before treatment and continuing for two weeks after. At MD Anderson Cancer Center, this helped 65% of patients.
Watch for side effects. Long-term high doses can lower copper levels. Talk to your doctor before starting. Don’t self-prescribe.
2. Change Your Utensils
It sounds silly, but metal spoons and forks can make the metallic taste worse. Why? They release tiny ions that mix with the drug residue in your saliva. Switch to plastic, bamboo, or glass utensils. Use ceramic plates. It’s a small change-but people on the PatientsLikeMe platform report noticing a difference within days.
3. Eat Tart or Sour Foods
Acidic flavors like lemon, lime, pickles, or vinegar stimulate saliva and override the metallic sensation. Try squeezing a wedge of lemon over your food before eating. Or suck on a sugar-free lemon drop. One study in the Journal of Supportive Oncology found this simple trick improved food enjoyment in over half of patients.
4. Marinate Your Protein
Plain chicken or fish tastes like cardboard when you have dysgeusia. But marinate it in strong flavors-teriyaki, barbecue sauce, garlic-herb blends, or even a splash of soy sauce and ginger. The bold taste overpowers the metal. Freeze-dried fruits like mango or pineapple can also reset your palate between bites.
5. Take Medication With Food
For drugs like Paxlovid, taking them on an empty stomach makes the taste worse. The FDA found that taking it with a high-fat meal reduces metallic taste complaints by 27%. Eat a small sandwich, a spoonful of peanut butter, or some avocado before your dose. It slows absorption and lessens the drug’s direct impact on your tongue.
6. Boost Oral Hygiene
Brush your tongue twice a day-not just your teeth. Use baking soda toothpaste. It’s mildly alkaline and helps neutralize the acidic environment that makes metallic taste stick around. Floss daily. Plaque buildup can trap drug residues and make the problem worse. Get a professional cleaning every 3-4 months if you’re on long-term meds.
What Your Doctor Can Do
You shouldn’t have to suffer silently. Here’s what to ask for:
- Can we check my zinc levels? A simple blood test takes minutes.
- Is there a similar medication without this side effect? For example, if you’re on an ACE inhibitor like lisinopril and get metallic taste, switching to an ARB like losartan might help.
- Can we lower the dose? Sometimes, reducing the dose slightly reduces taste distortion without losing effectiveness.
- Are there new formulations? In January 2023, the FDA approved a new lithium carbonate tablet with a polymer coating that cuts metallic taste by over 65%. Ask if newer versions exist for your drug.
Pharmaceutical companies are finally listening. New taste-masking tech like Geomelt® a delivery system that coats iron supplements to prevent metallic taste and Lipocure a lipid-based system used to reduce metallic taste in chemotherapy drugs are now in use. These aren’t sci-fi-they’re real, available options.
When to Worry
Most cases of drug-induced dysgeusia aren’t dangerous. But if you also have:
- Complete loss of taste for more than two weeks
- Difficulty swallowing or pain in your mouth
- Unexplained weight loss or dehydration
-then see your doctor. These could signal something else, like a neurological issue or severe nutritional deficiency.

What’s Next for Treatment?
The science is moving fast. In 2023, researchers at the National Institutes of Health launched a $2.5 million project to study how drugs interfere with TRPM5 a key protein in taste cell signaling pathways. Early results suggest some people have a genetic vulnerability-specifically, variants in the TAS2R38 a gene linked to bitter taste sensitivity gene-that make them more likely to get metallic taste from certain drugs.
Soon, doctors may be able to test your DNA before prescribing and choose a drug that won’t mess with your taste. Until then, the tools we have now-zinc, tart foods, better hygiene, and talking to your provider-are enough to make a real difference.
Real Stories, Real Relief
A 72-year-old woman in Bristol started taking metronidazole for a dental infection. Within two days, she couldn’t eat meat or drink coffee. She lost 8 pounds in three weeks. Her doctor told her to "just wait it out." She found a pharmacist who suggested zinc. After 10 days on 50 mg daily, her taste returned. She started cooking again.
A cancer patient on carboplatin couldn’t eat red meat for three weeks after each cycle. She tried lemon wedges before meals, switched to plastic utensils, and started zinc. She gained back the weight she lost.
These aren’t miracles. They’re smart, simple fixes.
Can zinc supplements help with metallic taste from any medication?
Zinc can help if your metallic taste is linked to low zinc levels, which is common with antibiotics, chemotherapy, and aging. But not all cases are due to deficiency. For some drugs, the taste distortion comes from direct nerve or receptor interference. A 25-50 mg daily trial for 2-4 weeks is safe for most people and worth trying under medical supervision.
How long does metallic taste last after stopping a medication?
Usually, it fades within a few days to two weeks after stopping the drug. For some, especially after chemotherapy or long-term use of certain antidepressants, it can take up to a month. If it lasts longer than 30 days after stopping, see your doctor-it could point to another issue like nerve damage or chronic zinc deficiency.
Does drinking water help with metallic taste?
Plain water doesn’t usually help much. But sipping cold water between bites can rinse away drug residue and temporarily reset your taste. Adding lemon or mint can make it more effective. Avoid sugary drinks-they can make your mouth feel stickier and worsen the sensation.
Can I use mouthwash to fix metallic taste?
Avoid alcohol-based mouthwashes-they dry out your mouth and make taste problems worse. Instead, use a baking soda rinse: mix 1 teaspoon of baking soda in a cup of warm water. Swish gently, then spit. It neutralizes acids and cleans your tongue without irritation.
Should I stop taking my medication if I get metallic taste?
Never stop a prescribed medication without talking to your doctor. For some drugs-like antibiotics or blood pressure meds-stopping early can lead to serious complications. Instead, ask for alternatives, dose adjustments, or coping strategies. The goal is to keep you healthy without ruining your quality of life.
Are children more likely to get metallic taste from medications?
Children are actually more sensitive to unpleasant tastes, which is why the FDA now requires taste testing for all new oral medications meant for kids. About 42% of children refuse necessary medicines because of bad taste. While metallic taste is less commonly reported in children than in adults, the impact is bigger-they’re more likely to refuse to take the drug at all.
What to Do Next
If you’re dealing with metallic taste right now, start with three simple steps:
- Check if you’re on a known offender-antibiotics, lithium, ACE inhibitors, or chemotherapy drugs.
- Start a zinc supplement (25-50 mg daily) and switch to plastic utensils.
- Call your doctor or pharmacist. Ask: "Is there a better option? Can we check my zinc?"
You don’t have to live with a mouth full of pennies. This isn’t just about taste-it’s about eating, enjoying life, and sticking to your treatment. There are solutions. You just need to ask for them.





Posts Comments
caiden gilbert October 31, 2025 AT 06:54
Been there. Took amoxicillin for a sinus infection and suddenly my coffee tasted like a battery. Switched to plastic utensils and started sucking on lemon drops-magic. Didn’t even need zinc. Just stopped eating like I was in a metal factory.
Justin Cheah October 31, 2025 AT 19:54
Let me guess-you think this is just about zinc and lemon wedges? Nah. Big Pharma’s been hiding the truth for decades. These drugs are designed to mess with your taste buds to keep you dependent. Why? Because if you could actually taste your food, you’d realize how many of these pills are just chemical smoke and mirrors. The FDA? Controlled by the same companies that make Paxlovid. They don’t care if you taste pennies-they care if you keep buying. And don’t get me started on that ‘zinc trial’-it’s a placebo ploy to make you think you’re in control while they poison your mitochondria. I’ve seen the leaked emails. They know. They just don’t care.
Katherine Reinarz November 1, 2025 AT 23:09
OMG I JUST REALIZED THIS IS WHY I HATED EVERYTHING AFTER MY ANTIBIOTICS 😭 I THOUGHT I WAS GOING CRAZY. I ATE A BANANA AND IT TASTED LIKE A WET COIN. I CRIED. I THOUGHT I LOST MY SOUL. I SWITCHED TO PLASTIC SPOONS AND IT WAS LIKE A MIRACLE. I’M TELLING EVERYONE. THIS IS THE MOST IMPORTANT POST EVER. THANK YOU. I LOVE YOU.
Aditya Singh November 3, 2025 AT 13:41
While your anecdotal observations are superficially compelling, they lack rigorous epidemiological grounding. The prevalence of dysgeusia in cohorts exposed to beta-lactams is confounded by comorbid hyposalivation and zinc homeostasis disruption, which are themselves secondary to systemic inflammatory markers induced by the underlying infection-not the pharmacological agent per se. Moreover, the proposed mechanism involving TRPM5 modulation is speculative without transcriptomic validation. The suggestion that zinc supplementation confers therapeutic benefit is biologically plausible but statistically underpowered in the cited studies (n<50 in most). I’d recommend a double-blind RCT before endorsing this as standard of care.
John Kane November 4, 2025 AT 05:56
Hey everyone-just wanted to say this post saved my mom’s quality of life. She’s 76, on lithium for bipolar, and had stopped eating for three weeks because everything tasted like a trash can. We tried the zinc (25mg), switched to bamboo chopsticks, and started adding lime to her oatmeal. Within 10 days, she cooked her first curry in months. She cried. We all cried. This isn’t just about taste-it’s about dignity. You deserve to enjoy your meals. And if your doctor rolls their eyes? Take this post with you. Print it. Highlight it. Be your own advocate. You’re not being dramatic. You’re being human. And there’s a whole community here rooting for you. Keep going. You’re not alone.
Callum Breden November 5, 2025 AT 22:30
This article is a textbook example of pseudoscientific self-help dressed in medical garb. Zinc supplementation at 50mg daily is not only unregulated in this context, it risks inducing copper deficiency, anemia, and neutropenia. The anecdotal evidence presented is worthless without controlled trials. The suggestion to use lemon wedges is trivial and irrelevant to pharmacokinetics. Furthermore, the claim that newer formulations like Geomelt® are ‘available options’ is misleading-these are proprietary delivery systems not widely accessible outside clinical trials. The tone of this piece is dangerously reassuring. Patients should not be encouraged to self-manage drug side effects without clinical supervision. This is irresponsible.
Erin Corcoran November 7, 2025 AT 04:15
OMG YES TO THE BAKING SODA RINSE!! 🙌 I’ve been using it since I started chemo and it’s been a game-changer. Also, the plastic utensils thing? SO TRUE. I used to hate my spoon so much I’d just eat with my hands. Now I feel like a gourmet chef with my bamboo fork 😄 Also-zinc helped me too! Just started 30mg, and my steak actually tasted like steak again. Thank you for writing this. I felt so alone until now 💛
Mansi Gupta November 9, 2025 AT 01:47
Thank you for sharing such a thoughtful and evidence-based overview. I work in geriatric pharmacy in Delhi, and we see this issue frequently among elderly patients on polypharmacy. Many dismiss it as aging, but it is often medication-induced. We now routinely screen for zinc levels and recommend tart foods as first-line intervention. The cultural aspect is also important-many patients avoid citrus due to traditional beliefs about ‘cooling’ foods, so we tailor suggestions carefully. Your mention of genetic variants in TAS2R38 is particularly valuable. We are beginning to integrate pharmacogenomics into our counseling. This is exactly the kind of practical, compassionate guidance our field needs.
Write a comment