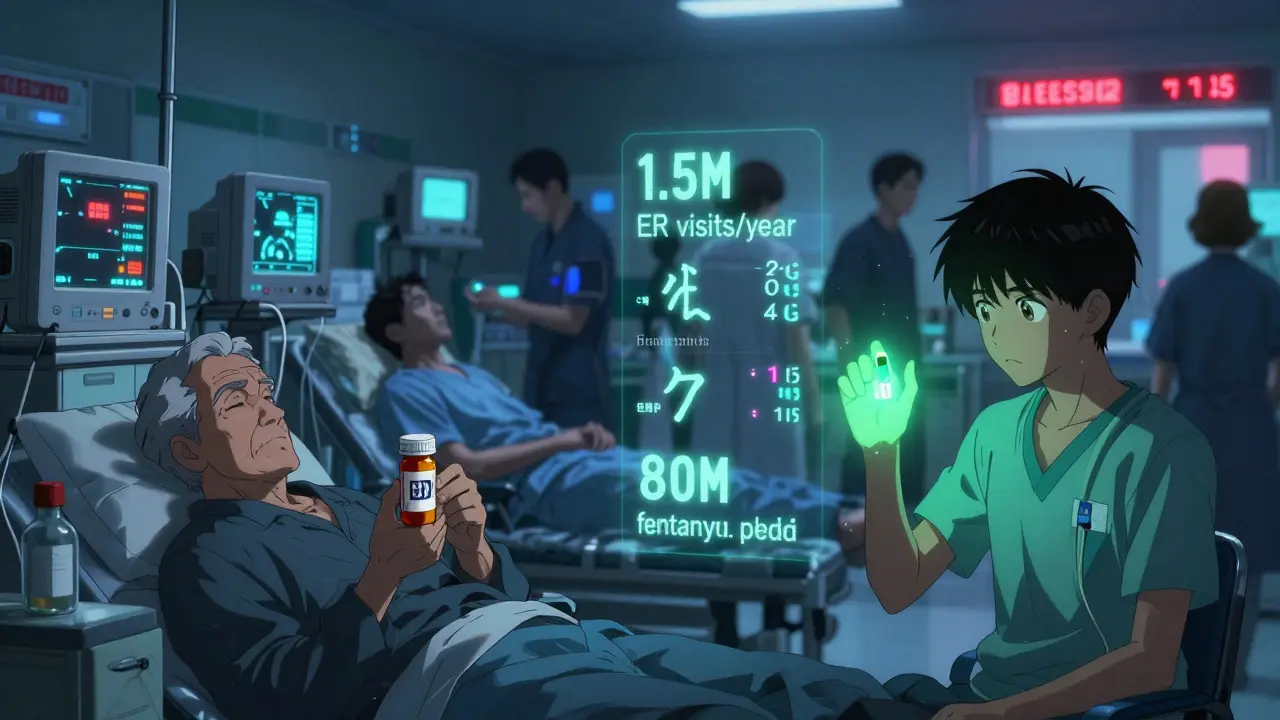
Every year, more than 1.5 million people in the U.S. end up in emergency rooms because of medication mistakes. These aren’t rare accidents-they’re preventable. And they’re happening to people you know: grandparents taking the wrong dose of blood pressure pills, teens overdosing on fake painkillers, new moms confused by discharge instructions. This isn’t just a hospital problem. It’s a public health crisis.
Medication Errors Are Killing People-And It’s Getting Worse
The World Health Organization says unsafe medication practices cause more harm than almost any other issue in healthcare. In high-income countries, one in ten patients suffers avoidable harm from a medication error. In lower-income places, it’s one in twenty. That’s not a glitch in the system-it’s the system itself failing.
Between 2020 and 2024, the number of days people spent on medication therapy jumped by 1.7%. That means more drugs, more prescriptions, more chances for something to go wrong. And it’s not just about dosage. Fentanyl-laced counterfeit pills seized by the DEA in 2023 alone totaled over 80 million. Fentanyl is now the leading cause of death for Americans between 18 and 45. These aren’t just drug overdoses-they’re medication safety failures. People thought they were taking oxycodone. They got poison.
The CDC reports that adverse drug events send more people to the ER than falls, car crashes, or infections. And the cost? Over $42 billion globally every year. In the U.S., medication non-adherence alone causes $300 billion in avoidable spending and kills 125,000 people annually. That’s more than traffic accidents. More than breast cancer. And most of it is preventable.
It’s Not the Doctors-It’s the System
Most people assume medication errors happen because someone made a mistake. A nurse misread a label. A pharmacist miscounted pills. A doctor wrote the wrong dose. But research shows something different. A 2024 study in JAMA Internal Medicine found that 89% of errors come from system flaws-not human carelessness.
Look-alike, sound-alike drug names. Confusing EHR interfaces. Poor communication between hospitals and pharmacies. Discharge instructions written in medical jargon. These aren’t accidents. They’re design failures. Nurses on Reddit reported that 68% of them had a near-miss error every month because two drugs looked identical on the screen. Pharmacists said 43% of errors they caught were caused by EHRs that didn’t flag dangerous interactions.
Even when technology is in place, it doesn’t always help. A 2024 analysis of 15,000 patient transitions found that 67% of people had at least one unintentional change in their medication when moving from hospital to home. One patient was discharged on warfarin but never got the lab test to monitor it. Another was told to stop a drug they’d been on for ten years-without a plan to replace it. These aren’t rare. They’re routine.
Technology Can Save Lives-If It’s Done Right
There are proven fixes. Barcode-assisted medication administration (BCMA) cuts administration errors by 86%. Electronic prescribing with clinical decision support reduces mistakes by 55%. AI tools can now predict which patients are at highest risk for adverse events with 73% accuracy.
The Mayo Clinic used AI to reconcile medications after discharge and slashed post-hospital errors by 52%. Geisinger Health’s pharmacist-led program boosted adherence to 89% for chronic conditions and cut readmissions by 27%. These aren’t theoretical. They’re happening now.
But adoption is uneven. While 94% of U.S. hospitals use barcode systems, only 63% use them well enough to make a real difference. Independent doctors’ offices? Only 42% have any structured safety program. Rural hospitals? Just 37% offer 24/7 pharmacist support. Meanwhile, top-performing systems-like the Netherlands’ national electronic prescribing network-cut errors by 44% by forcing everyone to use the same system.

Why the U.S. Is Falling Behind
The U.S. spends more on healthcare than any country. But we don’t lead in safety. We lag.
Only 38 states require pharmacy technicians to be certified. There’s no national standard for reporting medication errors. Only 14% of errors are ever formally reported. That means we’re flying blind. The FDA’s MAUDE database tracks 204,163 infusion pump incidents in 18 months-including 204 deaths. But without mandatory reporting, we can’t fix what we don’t measure.
Compare that to the UK. Their National Reporting and Learning System collects every near-miss and error. That data feeds into training, policy, and system redesign. Result? A 30% drop in serious medication errors. No magic. Just accountability.
And then there’s the drug supply. The FDA’s new DSCSA rule, fully in effect by November 2025, will require electronic tracking of every prescription package. That’s huge. But it’s late. Counterfeit drugs are growing 25% a year. We’re fighting the future with yesterday’s tools.
Patients Are the Weakest Link-And the Strongest Solution
Medication safety isn’t just about doctors and tech. It’s about patients understanding what they’re taking. A 2024 survey found 76% of patients had trouble communicating about their meds during hospital stays. 32% didn’t understand their discharge instructions.
Simple fixes work. Visual medication schedules reduced errors by 38%. Patient portals that show drug names, doses, and reasons increased adherence by 29%. Pharmacist-led check-ins boosted adherence by 40% and saved $1,200 per patient per year.
The WHO says improving adherence has a bigger impact on population health than any single drug. That’s not a slogan. It’s data. If 10% more people took their blood pressure meds correctly, we’d prevent tens of thousands of strokes. If 10% more people took their diabetes drugs as prescribed, we’d cut kidney failure and amputations dramatically.

What Needs to Change-And How
This isn’t about blaming individuals. It’s about redesigning systems. Here’s what needs to happen:
- Mandatory national reporting of all medication errors-not just voluntary ones.
- Standardized training for pharmacy techs and nurses across all 50 states.
- Interoperable EHRs that talk to each other, not just within a hospital but between pharmacies, clinics, and homes.
- AI-powered alerts that don’t just warn about interactions, but predict who’s likely to miss doses or have a reaction.
- Pharmacist integration into primary care teams-not as refill clerks, but as medication safety experts.
- Clear patient instructions written in plain language, with visual aids, not just paper handouts.
The ROI is undeniable. Every dollar spent on medication safety returns $7.50 in savings. Pharmacist-led programs? $13.20 back. That’s not a cost. It’s a profit center.
The Bottom Line
Medication safety isn’t a side issue. It’s not a checklist item. It’s the foundation of healthcare. If we can’t get the right drug to the right person at the right time, nothing else matters.
We have the tools. We have the data. We have the proof that change works. What’s missing is the will. Until we treat medication safety like a public health emergency-with funding, standards, accountability, and urgency-we’ll keep seeing the same headlines: another death. Another ER visit. Another family shattered by something that never should have happened.
The numbers don’t lie. The stories don’t lie. The solution isn’t complicated. It’s just hard. And it’s long overdue.





Posts Comments
Luke Trouten February 12, 2026 AT 17:05
It's sobering to consider that medication safety failures are statistically more lethal than car crashes and breast cancer combined. What's striking isn't the scale of the problem-it's how little systemic urgency there is to fix it. We optimize for profit, convenience, and bureaucratic inertia, not human outcomes. The fact that 89% of errors stem from system design, not human error, should be a wake-up call. We don’t need more training-we need better architecture. And yet, the architecture remains unchanged because change is expensive and inconvenient. The real tragedy isn’t the deaths. It’s that we knew this was coming, and we still chose not to act.
Write a comment