Leprosy Treatment Duration Calculator
Leprosy treatment duration depends on the type of disease you have. Paucibacillary cases (low bacterial load) require shorter treatment than multibacillary cases (high bacterial load). This calculator helps determine your treatment timeline based on your classification.
Treatment Duration
This duration is based on WHO-recommended multidrug therapy (MDT) which includes dapsone, rifampicin, and clofazimine.
When most people think of Leprosy a chronic infection caused by the bacterium Mycobacterium leprae, they picture distant villages in Asia or South America. In reality, the disease still turns up on U.S. soil, albeit in very small numbers. This article unpacks why leprosy remains a public‑health curiosity in America, how cases are detected, what modern therapy looks like, and where patients can find help.
Historical Overview: From Arrival to Elimination Efforts
Leprosy, also known as Hansen's disease, arrived in North America with European colonists in the 1600s. Early records describe isolated patients living in “leper colonies” such as the one on Carville, Louisiana, which operated from 1894 to 1999. By the mid‑20th century, the World Health Organization (WHO) launched a global campaign to curb transmission, and the United States followed suit with a national surveillance program headed by the Centers for Disease Control and Prevention (CDC).
These initiatives dramatically lowered case counts. In 1980 the CDC reported an average of 100 new cases per year. By 2000 that number dropped below 50, and today the disease is classified as “rare but persistent.”
Epidemiology in the United States: Numbers That Matter
According to the latest CDC data (2023), the United States records roughly leprosy United States 150 new diagnoses every five years. While that sounds tiny compared to the millions living with chronic diseases, each case carries a hefty social and medical burden.
| Decade | Confirmed Cases | Most Affected States |
|---|---|---|
| 1990‑1999 | 473 | California, Texas, New York |
| 2000‑2009 | 322 | Florida, Louisiana, Hawaii |
| 2010‑2019 | 212 | California, Texas, Arizona |
| 2020‑2024 | 98 | California, New Mexico, Nevada |
The concentration in coastal and southern states mirrors the distribution of immigrant populations from endemic regions such as Brazil, India, and the Philippines. Importantly, there is no evidence of sustained person‑to‑person spread within U.S. communities; most infections are diagnosed years after exposure abroad.
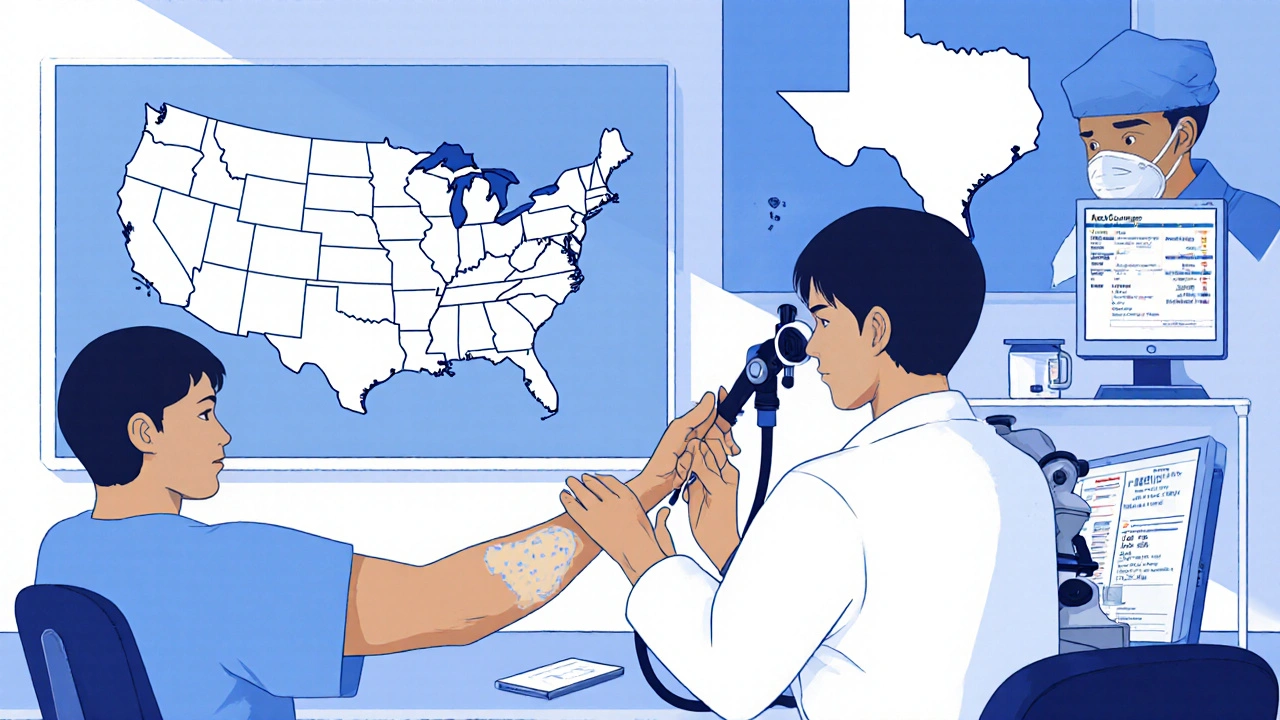
Symptoms & Diagnosis: Spotting the Subtle Signs
Leprosy’s hallmark is skin and nerve involvement. Early lesions may appear as pale, numb patches that resist normal sensation testing. Peripheral nerves-especially those near the elbows, knees, and earlobes-can thicken, leading to muscle weakness and loss of grip. Because these signs mimic other dermatologic conditions, clinicians rely on a combination of history, physical exam, and laboratory confirmation.
A definitive diagnosis hinges on a skin biopsy examined under a microscope for acid‑fast bacilli. PCR testing for Mycobacterium leprae DNA has improved sensitivity, especially in paucibacillary (low‑bacterial‑load) cases. The CDC also offers a reference laboratory that can confirm ambiguous specimens.
Treatment & Management: Modern Multidrug Therapy
Since the 1980s, the WHO‑endorsed multidrug therapy (MDT) has been the gold standard. MDT combines dapsone, rifampicin, and clofazimine for 6‑12 months, depending on disease classification (paucibacillary vs. multibacillary). This regimen kills the bacteria, stops transmission, and dramatically reduces the risk of disability.
For patients who develop nerve inflammation-known as reversal reactions-physicians may add a short course of corticosteroids. Early intervention is critical to preserve hand and foot function. Physical therapy, custom orthotics, and patient education further help prevent permanent deformities.
Because leprosy is not curable in the sense of eradicating every bacterial remnant, lifelong follow‑up is recommended to monitor for relapse or late reactions.
Public Health Response: Surveillance, Stigma Reduction, and Support
The CDC’s leprosy surveillance system captures each new case, assigns a unique identifier, and tracks treatment outcomes. Data are shared with state health departments to ensure rapid access to MDT and to coordinate contact‑tracing when necessary-though true contacts are rare.
Stigma remains a major barrier. Historically, leprosy patients faced forced isolation, a legacy that still fuels fear. Public‑health campaigns now emphasize that leprosy is **not** highly contagious and that successful treatment renders patients non‑infectious within weeks.
Patient advocacy groups-such as the American Leprosy Missions-provide counseling, financial aid for medication, and community networking. These services are essential, especially for immigrants who may lack insurance.

Common Misconceptions: Debunking Myths
- Myth: Leprosy spreads through casual contact. Fact: Transmission requires prolonged exposure to untreated nasal secretions from an infectious person.
- Myth: A single bite of an insect can cause leprosy. Fact: The exact environmental reservoir is unclear, but armadillos can harbor the bacterium in some U.S. regions; however, human‑to‑human transmission is far more common than zoonotic spread.
- Myth: Leprosy is always fatal. Fact: With MDT, cure rates exceed 95 % and patients can lead normal lives.
How to Get Help: Steps If You Suspect Leprosy
- Contact your primary care physician or a dermatologist as soon as you notice persistent numb patches or nerve thickening.
- Ask for a referral to a leprosy specialist; many are located at university medical centers in California, Texas, and Florida.
- Ensure the clinician orders a skin biopsy and, if available, PCR testing.
- If diagnosed, the CDC will provide free MDT through its National Leprosy Surveillance Program.
- Follow up regularly for at least two years to monitor for reactions and disability.
Never delay care out of fear of stigma-early treatment stops disease progression and alleviates anxiety.
Resources & Further Reading
For the most up‑to‑date information, consult these trustworthy sources:
- CDC Leprosy Page - case statistics and treatment guidelines.
- WHO Leprosy Fact Sheet - global perspective and historical data.
- American Leprosy Missions - patient support and financial assistance.
Is leprosy still contagious in the United States?
Transmission is possible but rare. It requires prolonged, close contact with an untreated patient’s nasal secretions. Once MDT begins, patients become non‑infectious within weeks.
How long does multidrug therapy last?
Paucibacillary cases usually finish a 6‑month regimen; multibacillary cases require 12 months of MDT.
Can leprosy cause permanent disability?
If left untreated, nerve damage can lead to loss of sensation, muscle weakness, and deformities. Early diagnosis and prompt MDT greatly reduce this risk.
Are armadillos a source of leprosy in the U.S.?
Armadillos in some southern states harbor Mycobacterium leprae. Zoonotic transmission is possible but accounts for a small fraction of cases; human‑to‑human spread remains the primary route.
Where can I find free treatment?
The CDC provides MDT at no cost through its National Leprosy Surveillance Program. Contact your state health department for enrollment details.






Posts Comments
Giusto Madison October 21, 2025 AT 17:37
Look, the data on leprosy cases in the US is clear-it's rare but still shows up, so you can't afford to be complacent. Get checked early if you notice numb patches; the CDC's free MDT works fast. Don't wait for a myth to die down before you act; early treatment means zero transmission within weeks. Stay vigilant and spread the word, not the disease.
Xavier Lusky November 1, 2025 AT 08:27
The CDC and WHO are just the tip of an elaborate cover‑up. They want us to think leprosy is "rare" so they can keep their silent programs hidden. Every time they announce a new case, it's a reminder that something's not being told. Don't trust the official numbers-they're filtered through a lens of control.
Esther Olabisi November 12, 2025 AT 00:17
Wow, you read all that and still think leprosy is some sci‑fi monster 😏. Good thing modern MDT is a real thing, not a myth. If you ever feel a weird patch, just get a biopsy before you start panicking. Keep your head up, everyone’s got a chance to get treated and live normally! 😂
Vivian Annastasia November 22, 2025 AT 16:07
Sure, because the CDC is just handing out free meds with no strings attached, right? It's a classic case of "we care enough to give you the drugs, but not enough to fix the stigma." I guess if you love being a victim of history, you can stay in the shadows forever.
John Price December 3, 2025 AT 07:57
Sounds good.
Ericka Suarez December 13, 2025 AT 23:47
America's so great we even have leprosy but still manage to find a cure! The drama of it all is like a Hollywood script, only it's real and you can actually get help! Don't let the old stereotypes scare you, the CDC's got the drugs and they work!
Ivan Laney December 24, 2025 AT 15:37
Listen up, folks-when you read about leprosy showing up in the United States, you have to understand the bigger picture that most people choose to ignore. The disease's persistence is not some random fluke; it reflects the porous borders and the influx of immigrants from endemic regions, which our government continuously debates but never truly addresses. While the CDC claims it’s "rare but persistent," that language masks the fact that we still lack a comprehensive domestic surveillance program that reaches every community. We have the technology-PCR, skin biopsies, multidrug therapy-but we fall short on education, especially in rural clinics where the fear of stigma is still rampant. The historical leper colonies like Carville are gone, but the ghosts of that era linger, and the social stigma continues to deter people from seeking help. You think the MDT regimen is just a six‑to‑twelve‑month course? No, it's a public health commitment that demands continuous monitoring, physical therapy, and community support. If you skip the follow‑up, you risk nerve damage that can become permanent, turning a treatable condition into a lifelong disability. The real issue is not the bacteria, but how we, as a society, handle the narrative surrounding it. A lot of the public still believes the myth that casual contact spreads leprosy, which is why outreach programs are essential. The CDC’s free provision of MDT is commendable, yet it’s a band‑aid if we don’t simultaneously dismantle the prejudice. The environmental reservoirs, like armadillos, illustrate that disease ecology is complex, and snapping fingers at it without robust research is naïve. Moreover, the geopolitical dynamics of immigration policy influence the statistics we see-fewer reports don’t mean fewer cases. In short, the fight against leprosy in America is a microcosm of our broader healthcare challenges: we have the tools, but we lack the will to implement them fully across all demographics.
Kimberly Lloyd January 4, 2026 AT 07:27
It's encouraging to see that modern medicine can turn a disease once shrouded in fear into a manageable condition. Remember, early detection is a gift we give ourselves and our community. Let’s keep the conversation open and support those navigating the journey.
Sakib Shaikh January 14, 2026 AT 23:17
Behold! The drama of a disease that creeps across borders, yet we stand armed with miracles called multidrug therapy. Even the armadillo, that humble creature, carries the secret of the ancient pathogen, reminding us that nature loves a good plot twist.
Write a comment